Laryngeal Papillary Cystadenoma: A Case Report
Article information
Abstract
Papillary cystadenoma is a rare, benign salivary gland neoplasm containing cystic cavities with intraluminal papillary projections. In the head and neck area, it occurs mainly in major and intraoral minor salivary glands, but rarely in the larynx. We report a case of a 67-year-old female with a chief complaint of hoarse voice diagnosed as laryngeal papillary cystadenoma. This paper emphasizes the need to consider papillary cystadenoma as one of differential diagnosis when benign looking lesions are observed in the larynx, where it uncommonly occurs.
INTRODUCTION
Cystadenoma is a benign neoplasm which constitutes 0.7% to 8.1% of all benign salivary gland tumors. It is composed of multiple cystic spaces lined by variable epithelium with focal intraluminal papillary proliferations. The average age of occurrence is about 50 years with female predominance (female-to-male ratio, 3:1). Most of the cystadenomas arise in major salivary glands, 58% in parotid gland and 7% in submandibular gland. Minor salivary gland cystadenomas affect mostly the lip and buccal mucosa [1]. Minor salivary glands tumors are rarely observed in the larynx. They arise from the submucosal glands and constitute less than 1% of laryngeal tumors [2].
Herein we present a rare case of laryngeal papillary cystadenoma with its histologic features, diagnosis, and treatment process.
CASE REPORT
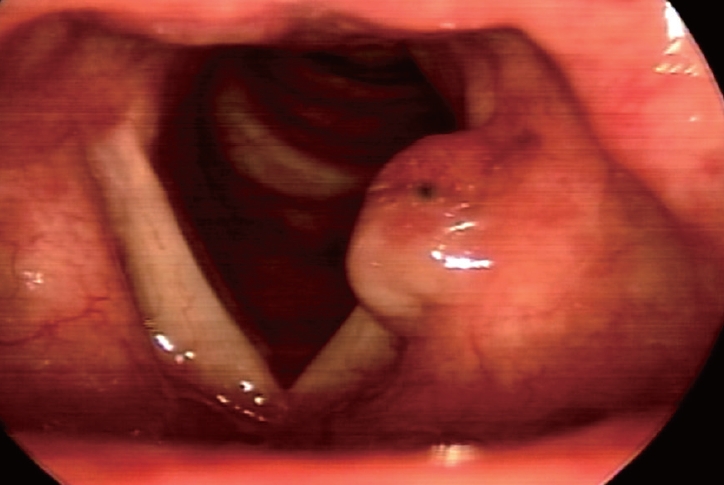
A 67-year-old female without remarkable medical history presented with chief complaint of hoarseness which started a month ago. There was no dyspnea, dysphagia nor odynophagia. Laryngeal examination with videostroboscopy revealed a submucosal benign looking granulomatous mass at her left false vocal fold. Both true vocal cords were normal in appearance and mobility. The subglottis was also free (Fig. 1). Routine blood tests were within normal limits. There was no palpable cervical lymphadenopathy. Computed tomography scan revealed approximately 7-mm-sized enhancing nodular lesion at left laryngeal ventricle. There was neither significant cervical lymphadenopathy nor other abnormality in the pharynx and salivary gland (Fig. 2).

Contrast-enhanced neck CT revealed approximately 7-mmsized enhancing nodular lesion in the laryngeal ventricle (arrows).
To excise and biopsy the supraglottic mass, laryngeal microsurgery was performed under general anesthesia. Kleinsasser laryngoscope was inserted for suspension exam of larynx. The well-circumscribed soft mass surrounded by granulation tissue was originating from left laryngeal ventricle. The mass was extending to left thyroarytenoid muscle. The supraglottic mass was completely excised using CO2 laser, with sufficient safety margin (Fig. 3). A frozen section biopsy identified the mass as a benign lesion. The remaining whole specimen was sent to pathologist for histopathological analysis.

Operative pictures of the supraglottic mass. A: The mass was extended to the ventricle and true vocal fold. B: Excision of the mass using CO2 laser. C: Postoperative status.
Histopathological analysis revealed submucosal multiseptated cystic lesion measuring 0.7 cm in the greatest diameter (Fig. 4A). The cyst was characterized by inner papillary projections, which were lined by columnar epithelial cells (Fig. 4B and C). The cells showed no significant cytologic atypia or mitotic figures (Fig. 4D), and no abnormal invasion into the fibrous capsule was noted. Therefore, the patient was finally diagnosed with papillary cystadenoma (PC).
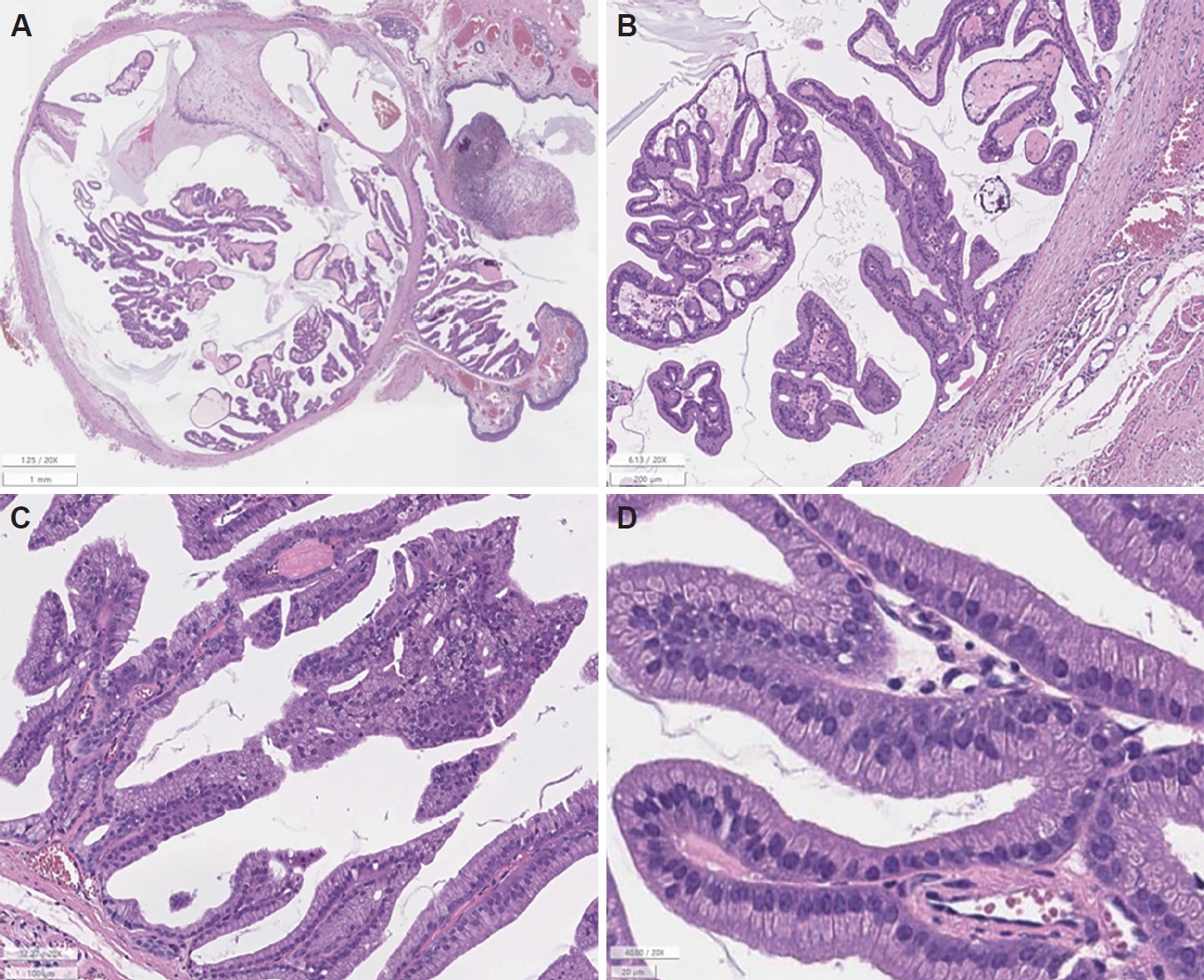
Histologic features (Hematoxylin-Eosin staining, ×20). A: Well-circumscribed multicystic lesion with papillary cores is noted on low power. B, C: Columnar cells with eosinophilic cytoplasm were lining the fibrovascular cores. D: The cells were uniform and bland-looking without any malignant features on magnified view.
Postoperative hospital course was uneventful. The patient was followed up for over 1 year with no evidence of recurrence.
DISCUSSION
As previously described, cystadenomas are rare, benign neoplasms. The rarity of PCs has been reported by many authors. A retrospective study of 6982 cases of salivary gland by Tian et al. [3] reported that cystadenomas account for 0.59% of benign salivary gland tumors and there was only one case of laryngeal cystadenoma out of 28 cases of cystadenomas. A review of 426 cases of intraoral minor salivary gland tumors by Waldron et al. [4] reported that PC comprises 4.7% of minor salivary gland tumors. PubMed and Google Scholar database search from 1953 to 2021 revealed only 4 cases of non-oncocytic laryngeal papillary cystadenoma in the English literature [5-8].
Histologically, cystadenomas consist of multicystic proliferation of glandular epithelium which could be oncocytic, apocrine, epidermoid, and mucinous. WHO classification (2005) of salivary gland tumors discriminated two variants of cystadenoma: papillary cystadenoma and mucinous cystadenoma [9]. Mucinous cystadenoma is composed of multiple cysts lined exclusively by mucinous cells. Papillary type cystadenoma as in this case is characterized by cystic lesion with intraluminal papillary projections. The lining epithelial cells may accompany oncocytic metaplasia which is suspected to be related with age and is facilitated by smoking [1]. However, in this case oncocytic change was not observed.
In the larynx, the most common anatomical site of cystadenoma is the supraglottis (74%). This is due to abundant distribution of seromucinous salivary glands in laryngeal ventricles and vestibular folds. Hoarseness is the most common symptom. Less frequent symptoms include globus, dysphagia, pain, stridor, and laryngeal obstruction [10].
In our case, laryngeal examination with videostroboscopy revealed the benign looking mass located at supraglottis. Further imaging work up with CT scan and/or MRI may give more information about the extent of the tumor and anatomical relationships. On CT, PCs appear as well defined, homogenous, isodense or slightly hyperdense, and smooth submucosal lesion [11].
The histopathological diagnosis is essential as many cystic lesions of the larynx are with similar property but requires different management. The differential diagnosis of PC involves papillary cystadenoma lymphomatosum (Warthin tumor), oncocytic cystadenomas, oncocytomas, low-grade mucoepidermoid carcinoma, cystadenocarcinoma, and intraductal papilloma.
The treatment of choice for laryngeal PC is complete excision with tumor-free margin as in the treatment of other benign tumors. Given the anatomical site and the size of the tumor, surgical approach could be made transorally or transcervically with endoscopic and/or microscopic assistance. The cases of oncocytic papillary cystadenoma accompanying squamous cell carcinoma have been reported [12]. However, these cases were extremely rare and malignant transformation of oncocytic cystadenoma has not been reported so far [13]. Although PC is a benign lesion, considering its possibility of recurrence and multiple site involvement [14,15], follow-up is recommended. In our case, annual visit was planned starting from 1 year after operation.
We present this rare case of laryngeal PC to emphasize that clinicians should consider this disease as one of the differential diagnosis of laryngeal cystic lesions. In addition, histopathological diagnosis is critical in diagnosing the PC as many salivary gland tumors show similar features. Curative treatment is complete surgical excision with tumor-free margin.
Acknowledgements
None.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Authors’ Contribution
Conceptualization: Seong Keun Kwon. Data curation: Min-Kyung Kim. Formal analysis: Min-Kyung Kim, Jiwon Koh. Investigation: Min-Kyung Kim, Seong Keun Kwon. Methodology: Min-Kyung Kim, Seong Keun Kwon. Project administration: Min-Kyung Kim, Seong Keun Kwon. Resources: Kyeong Cheon Jung, Seong Keun Kwon. Software: Min-Kyung Kim, Seong Keun Kwon. Supervision: Kyeong Cheon Jung, Seong Keun Kwon. Validation: Min-Kyung Kim, Jiwon Koh, Seong Keun Kwon. Visualization: all authors. Writing—original draft: Min-Kyung Kim.Writing—review & editing: Jiwon Koh, Kyeong Cheon Jung, Seong Keun Kwon. Approval of final manuscript: all authors.