Comparison of Voice Outcomes Between Minimally Invasive Open Hemithyroidectomy and Conventional Hemithyroidectomy
Article information
Abstract
Background and Objectives
Voice change after thyroidectomy is a common complication that affects a patient’s quality of life. In this study, we aimed to compare voice outcomes between minimally invasive open hemithyroidectomy (MIOT) and conventional hemithyroidectomy.
Materials and Method
We enrolled 215 patients who underwent hemithyroidectomy performed by an experienced surgeon at our institute between June 2017 and December 2021. All patients underwent voice evaluations, including subjective and objective assessments, preoperatively and 2 weeks and 2 months postoperatively.
Results
Sixty-one patients underwent MIOT (M group) and 154 patients underwent conventional hemithyroidectomy (C group). There were 50 female (82.0%) and 11 male (18.0%) in the M group, and 129 female (83.8%) and 25 male (16.2%) in the C group. In both groups, the thyroidectomy-related voice questionnaire score increased at 2 weeks and 2 months postoperatively. However, no statistically significant differences were observed between the two groups. Voice parameters were analyzed according to sex. There were some changes in the parameters in both groups. However, no statistically significant differences were observed between the two groups.
Conclusion
Our study showed no differences in the acoustic results between MIOT and conventional hemithyroidectomy.
INTRODUCTION
Thyroidectomy is one of the most commonly performed surgeries worldwide. Since Theodor Kocher devised the conventional thyroidectomy in the late 19th century, mortality and morbidity have dramatically decreased because of the development of sensitive dissection and antisepsis techniques. This technique remains the standard approach for thyroid surgery [1].
Since the 1980s, minimally invasive surgical techniques have attracted interest in all surgical fields, including abdominal, thoracic, and head and neck surgeries. In thyroid surgery, cosmetic aspects are among the most significant concerns for patients, which has resulted in the recent appearance of various minimally invasive thyroid surgery (MITS) techniques. MITS can be divided into three types: mini-incision open, video-assisted, and complete endoscopic or robotic. Common features of each approach are the use of a small central or remote incision and alternative energy sources for hemostasis [2].
The frequency of hemithyroidectomy is increasing due to the latest changes in the American Thyroid Association Guidelines [3]. Minimally invasive surgical techniques are used more often in hemithyroidectomies than in total thyroidectomies. A minimally invasive open thyroidectomy involves a small central cervical incision. It has a similar morbidity to conventional thyroidectomy and has advantages in terms of patient satisfaction with scarring, reduction in postoperative pain, and hospital stay [2,4].
Although thyroid surgery is associated with low morbidity, postoperative voice changes are common. The main cause of voice changes after thyroid surgery is an injury to the recurrent laryngeal nerve (RLN) and external branch of the superior laryngeal nerve (EBSLN) during surgery [5]. However, many patients complain of voice disturbances despite no obvious nerve injury during thyroid surgery. The causes include orotracheal intubation injury, postoperative adhesions, and psychological factors [6]. In several studies, reports of subjective voice changes varied from 37% to 87%, and patients complained of vocal strain, difficulty with high-pitched vocalizations, and a harsh voice [6,7].
According to one study, voice changes in patients who underwent total thyroidectomy were significantly greater than those in patients who underwent thyroid lobectomy. We believe that the extent of surgery may affect the voice postoperatively. Therefore, MITS may have a voice-change sparing advantage because its surgical range is generally smaller than that of conventional thyroidectomy. Although many studies have shown that MITS shows superior results compared to conventional thyroidectomy in terms of cosmetic effects and postoperative pain reduction, there are few comparative studies on voice disorders.
In this study, we compared and analyzed the acoustic results of the patients who underwent conventional hemithyroidectomy with the acoustic results of those who underwent minimally invasive open hemithyroidectomy (MIOT). A thyroidectomy-related voice questionnaire (TVQ) and acoustic analysis were used to evaluate voice function.
METHODS
Participants
The data of 487 patients who underwent hemithyroidectomy performed by an experienced surgeon at our institution between June 2017 and December 2021 were reviewed. A total of 80 patients underwent MIOT (M group) and 407 patients underwent conventional hemithyroidectomy. There were no differences in the surgical indications between the two groups. A total of 180 patients were selected from the 407 patients who underwent conventional hemithyroidectomy using a stratified random sampling method considering age and sex (C group). For a sufficient sample size, 180 patients, 2.25 times the M group, were sampled. All patients underwent the same preoperative (1 day before surgery) and postoperative (2 weeks and 2 months after surgery) voice evaluations. Each evaluation included fiberoptic laryngoscopy, acoustic analysis, and TVQ.
The inclusion criteria were as follows: 1) micropapillary thyroid cancer on biopsy and 2) conventional hemithyroidectomy or MIOT. The exclusion criteria were as follows: 1) laryngeal disorders on preoperative or postoperative laryngoscopy (e.g., vocal cord palsy, vocal cord polyp, Reinke’s edema, and vocal cysts); 2) previous head and neck surgery, including thyroidectomy; 3) other than micropapillary thyroid cancer on biopsy; and 4) failure to complete all preoperative and postoperative voice evaluations.
Based on the exclusion criteria, 19 and 26 patients in each group were excluded from the analysis. Finally, 61 patients in the M group and 154 patients in the C group were included in the study.
IRB approval by Pusan National University Hospital Clinical Research Information System (IRB No. 2203-029-113).
Operative technique
MIOT was performed through a 3–4 cm horizontal cervical incision and backdoor approach. After induction of general anesthesia, the patient was placed in the supine position with the neck extended. A 3–4 cm unilateral skin incision was made along the skin crease, one finger breadth above the clavicle (Fig. 1A). After the platysma transection, the anterior border of the sternocleidomastoid muscle (SCM) was identified and laterally retracted. The lateral edges of the strap muscles were identified and retracted medially to expose the underlying thyroid gland (Fig. 1B). Branches of the superior thyroid artery and vein were individually exposed and ligated as closely as possible to the upper pole by retracting the thyroid gland inferiorly and medially. The middle thyroid vein was divided and ligated with a medial rotation of the gland (Fig. 1C). Subsequently, the rest of the thyroid lobe was easily dissected and retracted medially to facilitate identification of the RLN and parathyroid glands (Fig. 1D). The inferior thyroid veins were ligated and divided, and the thyroid lobe was freed from attachment to the ligament of Berry and underlying tracheal rings. The isthmus was transected and the dissected lobe was removed from the surgical field as a specimen [8].

Surgical procedure of minimally invasive open hemithyroidectomy (MIOT). MIOT was performed through cervical incision and backdoor approach. A 3–4 cm unilateral skin incision was made along the skin crease (A). Expose the thyroid gland by retracting the strap and sternocleidomastoid muscle (B). Dissection of the thyroid gland and ligation of the branches of the thyroid artery and vein (C). Identification of recurrent laryngeal nerve by retracting the thyroid lobe medially (D).
Conventional hemithyroidectomy was performed through a 6–8 cm horizontal cervical incision with one finger breadth above the clavicle. After transection of the platysma, the subplatysmal flaps were elevated to the level of the thyroid notch superiorly and the clavicle and sternum inferiorly. The strap muscles were separated vertically at the midline and retracted laterally to expose the thyroid gland. The gland was removed in a manner similar to that described above [9].
TVQ
The TVQ is a simple and effective screening tool for detecting pre- and post-thyroidectomy-related voice disorders that affect voice quality. The TVQ consists of 20 questions, and the TVQ score ranges from 0 (no voice alterations or symptoms) to 80 (greatest voice impairment with multiple vocal symptoms). The questions addressed general voice complaints, laryngopharyngeal reflux, vocal cord palsy, lower-pitched voices, and swallowing disorders associated with thyroidectomies [5]. At each of the three time points (pre-thyroidectomy and 2 weeks and 2 months post-thyroidectomy), the participants completed the TVQ. The total TVQ score was analyzed.
Voice recording and acoustic analysis
All voice samples were recorded in a soundproof booth (44 kHz sampling rate, 16 bits) with a unidirectional dynamic microphone (Shure SM48; Shure Inc., Chicago, IL, USA). The microphone was placed approximately 15 cm from the speaker’s mouth at an approximate angle of 15° to minimize the noise. The speaking tasks were to produce vowel sounds, including /a:/, /e:/, /i:/, /o:/, and /u:/ phonations, for 3 s and read Korean sentences from the “Sanchaek (a walk)” passage containing 69 syllables at comfortable pitch and loudness. Acoustic voice analysis was performed using the Multi-Dimensional Voice Program (MDVP, model 5105; KayPENTAX, Lincoln Park, NJ, USA) and Voice Range Profile program (VRP, model 4326; KayPENTAX) of the Computerized Speech Lab (CSL model 4500; KayPENTAX, Lincoln Park, NJ, USA). The voice parameters considered in the analysis were fundamental frequency (F0), speaking F0 (SFF), perturbations of frequency (jitter) and amplitude (shimmer), noise to harmonics ratio (NHR), VRP, and maximum phonation time (MPT).
Statistical methods
Statistical analyses were conducted using SPSS software version 22 (IBM Corp., Armonk, NY, USA). The t-test, chi-squared test, and Fisher’s exact test were used to analyze the outcomes. Changes in TVQ scores and voice parameters over time within the groups were assessed using paired t-tests. Comparisons between the groups were performed using independent t-tests. Statistical significance was set at p-value <0.05.
RESULTS
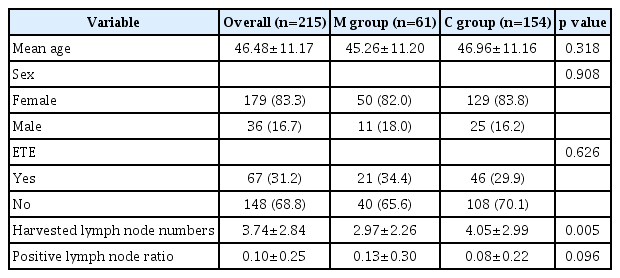
On the basis of the inclusion and exclusion criteria, 215 patients were included in this study. A total of 61 patients were enrolled in the MIOT group (M group). The mean age of the study population was 45.26±11.20 years. This group included 50 female patients (82.0%) and 11 male patients (18.0%). A total of 154 patients were enrolled in the conventional hemithyroidectomy group (C Group). The mean age of the study population was 46.96±11.16 years. Of them, 129 were female (83.8%) and 25 male (16.2%).
The characteristics of all the enrolled patients are shown in Table 1.
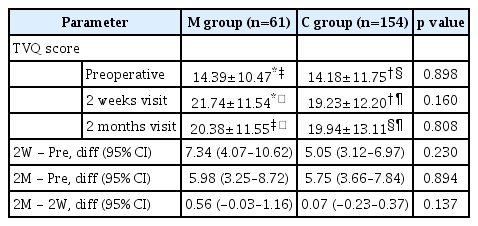
Preoperative and postoperative changes in the TVQ score
In both groups, the TVQ score increased at 2 weeks and 2 months postoperatively. There were no significant changes in TVQ scores between 2 weeks and 2 months in either group. In the M group, the TVQ scores of the male patients were 21.00±10.14 in 2 weeks and 18.36±10.27 in 2 months, and those of the female patients were 21.90±11.92 in 2 weeks and 20.82±11.87 in 2 months. In the C group, the TVQ scores of the male patients were 17.48±12.65 in 2 weeks and 18.88±12.54 in 2 months, and those of the female patients were 19.57±12.13 in 2 weeks and 20.14±13.26 in 2 months. A few differences were observed between the groups according to sex. There were no statistically significant differences between the two groups (Table 2).
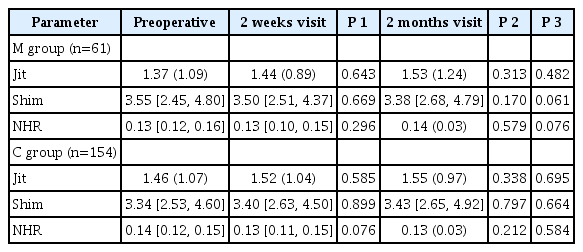
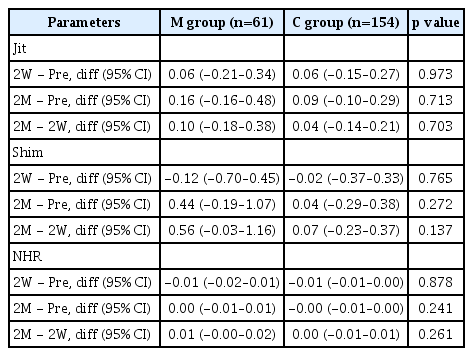
Preoperative and postoperative changes in the acoustic analysis
In both groups, jitter increased at 2 weeks and 2 months postoperatively; however, the change was not statistically significant. There were no statistically significant changes in the shimmer or NHR scores in either group (Tables 3 and 4). Because the analysis of the other voice parameters was different between male and female patients, we analyzed this according to sex.
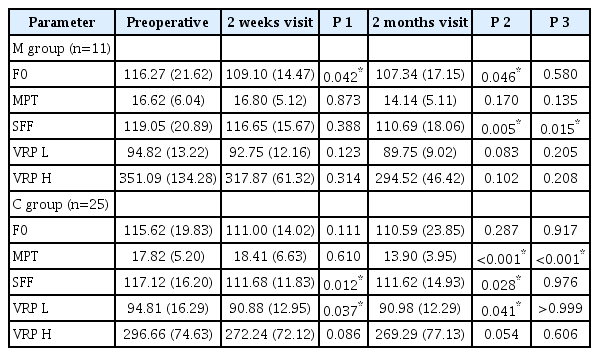
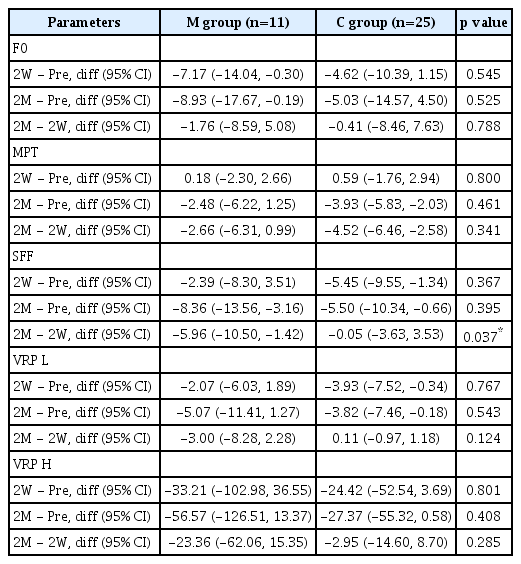
Male patients
Acoustic analysis in the M group showed that F0 decreased at 2 months postoperatively (p=0.042, p=0.046) and SFF decreased at 2 months postoperatively (p=0.005). The acoustic analysis in the C group showed that the SFF and VRP L decreased at 2 weeks postoperatively (p=0.012, p=0.037) and remained constant until 2 months postoperatively (p=0.028, p=0.041). There were no statistically significant differences between the two groups (Tables 5 and 6).
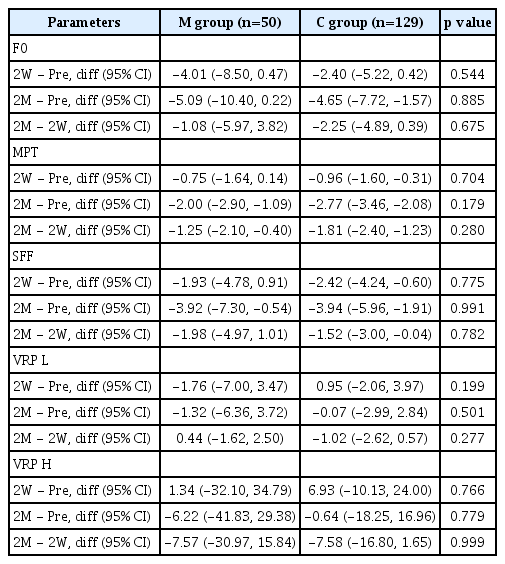
Female patients
Acoustic analysis in the M group showed that the MPT and SFF decreased 2 months postoperatively (p<0.001, p=0.024). Acoustic analysis in the C group showed that F0 decreased at 2 months postoperatively (p=0.003) and MPT decreased at 2 months postoperatively (p=0.004, p<0.001). The SFF also decreased at 2 months postoperatively (p=0.010, p<0.001). There were no statistically significant differences between the two groups (Tables 7 and 8).
DISCUSSION
Voice disturbance is one of the common complications of thyroidectomy, and it is a factor that significantly affects the quality of life. The primary known causes are RLN and EBSLN injuries during surgery. However, as surgical techniques for the thyroid region have improved, the incidence of RLN injuries has decreased [10]. Nowadays, RLN and EBSLN injuries happen in 0.7%–13.3% and 5%–30% of the cases following thyroidectomy, respectively [7]. The complication rate, including RLN lesions, was less than 2% when performed by an experienced surgeon [11]. Nevertheless, many patients complain of voice discomfort after thyroidectomy. Post-thyroidectomy voice disturbances are common in patients with preserved nerve function, and the patients recover over time [7,12]. Lang et al. [6] reported that the incidence of vocal changes ranged between 29.7% and 87%, depending on the definition and timing of the assessment. Multiple factors, including orotracheal intubation trauma, laryngotracheal fixation with impaired vertical movement, strap muscle malfunction, postoperative adhesion, local neck pain, and psychological factors, may lead to these symptoms [6,13]. Considering the possible causes, it can be considered that the extent of surgery may affect the voice postoperatively because the larger the extent of surgery, the greater the tissue damage. Park et al. [14] analyzed the voices of 217 patients who underwent a thyroidectomy. Voice changes were significantly greater in patients who underwent total thyroidectomy than in those who underwent thyroid lobectomy. Other studies have reported similar results [6,15].
In MITS, several procedures have been developed based on small incisions using various instruments and approaches. There are two main methods of MITS that use the mini-incision open technique. The first is to use the Sofferman technique after a mini cervical incision, that is, the method of transection of the strap muscle and immediate exposure of the thyroid gland [9]. The second method was performed in this study by approaching the thyroid gland using a backdoor approach after a mini cervical incision. Although there is a slight difference in the approach, these two methods use a similar surgical method overall, and there is no significant difference in the surgical results and complications. As described above, the MIOT uses a small incision and is designed to minimize tissue trauma by avoiding unnecessary tissue dissection while maintaining adequate exposure [8]. Therefore, MIOT has a relatively small surgical range compared to conventional thyroidectomy. Therefore, in addition to the known advantages of improved cosmesis, less postoperative pain, and shorter hospitalization period, this study was conducted with the assumption that MIOT may also have advantages in voice changes [4].
One study showed improved preservation of voice quality in patients undergoing minimally invasive video-assisted thyroidectomy compared to those undergoing conventional thyroidectomy [2]. With the introduction of the Da Vinci robot, surgeons have developed robot-assisted thyroidectomies. Among the robot-assisted thyroidectomy approaches [facelift, transvestibular, and bilateral-axillary breast approaches], robot-assisted transaxillary thyroid surgery (RATS) is a popular method. RATS creates a working space after using an axillary incision, and then performs surgery after robot docking [16]. This approach is similar to the backdoor approach used in the present study. Similar to other MITSs, RATS has shown better results than conventional thyroidectomy, in terms of cosmetic satisfaction and postoperative pain. In one study, RATS was more effective than conventional thyroidectomy for voice preservation; however, in most other studies, there was no difference in postoperative voice change between the two surgical methods [17,18].
TVQ scores increased after thyroidectomy in both groups, as shown in many other studies [5,12]. However, there was no statistically significant difference between the two groups. The increase in the TVQ score was not small in the M group compared to that in the C group, and it was the same when comparing male and female patients separately. Our study showed that there was no significant difference between the two groups in terms of TVQ score and acoustic analysis.
Conventional hemithyroidectomy involves a long collar incision of 6–8 cm, raises wide skin flaps on the anterior neck, and opens the midline of the strap muscles to expose the thyroid gland. This conventional approach may cause a wide neck scar and tissue trauma. The MIOT uses a small lateral incision approximately 3–4 cm in length and approaches the thyroid gland between the anterior border of the SCM and the strap muscles. This approach does not require opening the midline of the strap muscles or raising skin flaps, which can damage the subcutaneous tissue and anterior neck. This can reduce laryngotracheal fixation, strap muscle malfunctions, and postoperative adhesions. This approach also has the advantage of less postoperative pain, which may affect the voice quality. Therefore, MIOT could be a superior technique for preserving voice quality after surgery compared to conventional hemithyroidectomy. However, no such outcomes were observed in the present study.
Unlike conventional hemithyroidectomy, structures may be injured during MIOT. The ansa cervicalis nerve is deep in the SCM and innervates the infrahyoid muscles. It comprises both superior and inferior roots. The superior root of the ansa cervicalis travels with the hypoglossal nerve and descends along the anterior wall of the carotid sheath. After the superior root gives rise to a branch to the superior belly of the omohyoid, sternothyroid, and sternohyoid muscles, it joins the inferior root arising from C2–3 [19]. MIOT uses a backdoor approach, which can injure the ansa cervicalis nerve. This restricts movement of the strap muscles, which also affects phonation. However, only a few studies have examined the relationship between the ansa cervicalis and phonation.
The phonatory function of the strap muscles is not well defined. These muscles elevate and depress the larynx, and may lengthen or shorten the vocal cords in certain head positions [20]. Through scar tissue formation, this results in laryngotracheal fixation with impaired vertical movement. This problem is more evident in the case of strap muscle division. However, functional deficits in strap muscles and scar formation may result from elongation and retraction without division. Notably, we routinely retract the strap muscles without sectioning them [13]. One study showed that the strap muscle division had little effect on voice, as measured subjectively or objectively [20].
The cause of voice disturbances in patients with preserved nerve function after thyroid surgery has not yet been clearly identified. Several factors are presumed to cause postoperative voice disturbances, and we believe that all of these factors may work synergistically. However, research has not been conducted on the extent to which each factor contributes to voice disturbances and is difficult to assess [10]. Therefore, strap muscle functional deficits and scar formation may have less of an effect on voice disturbances postoperatively than other factors.
One limitation of our study was its small sample size. In particular, the number of male patients was insufficient for group comparison. The second limitation of our study is that we did not use of videostroboscopy or cricothyroid electromyography to demonstrate EBSLN injury. The third limitation is that no aerodynamic tests other than the MPT were performed.
In conclusion, there were no differences in the acoustic results between MIOT and conventional hemithyroidectomy.
Acknowledgements
This work was supported by clinical research grant from Pusan National University Hospital in 2023.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Authors’ Contribution
Conceptualization: Sung-Chan Shin, Byung-Joo Lee. Data curation: Myeonggu Seo, Geun-Hyo Kim. Formal analysis: Jiwon Jang, Yong-Il Cheon. Methodology: Bo Hyun Kim, In Ju Kim, Byung-Joo Lee. Visualization: Jiwon Jang, Sung-Chan Shin. Supervision: Yong-Il Cheon, Sung-Chan Shin, Bo Hyun Kim, In Ju Kim, Byung-Joo Lee. Writing—original draft: Myeonggu Seo, Byung-Joo Lee. Writing—review & editing: Byung-Joo Lee. Approval of final manuscript: all authors.