AbstractAirway foreign body aspiration in children can lead to accidental death, due to the foreign body itself or the removal procedure. Depending on its location, removal of the foreign body can be challenging. Here, we present a case of successful removal of a foreign body from the left upper lobar bronchus via ventilating bronchoscopy with a rigid bronchoscope and Fogarty arterial embolectomy catheter. Tracheobronchial foreign bodies in locations that are difficult to reach with forceps, due to an acute angle or the small diameter of the pediatric bronchial tree, can be effectively removed with a Fogarty arterial embolectomy catheter.
INTRODUCTIONAlthough the mortality rate is decreasing due to progress in bronchoscopic techniques, asphyxiation due to the inhalation of foreign bodies is still one of the leading causes of accidental death among children aged less than 4 years. A foreign body can be located in the respiratory tract anywhere from the main trachea to the main bronchi, and even in segmental bronchi if the aspirated material is very small. According to many reports on airway foreign body aspiration in pediatric patients, foreign bodies are typically discovered at the main bronchus level, with only a small percentage being located in the trachea or deeper parts of the bronchial tree [1].
Considering the anatomy of the bronchial tree, cases of foreign bodies located in the left upper lobar bronchus are uncommon. The upper lobar bronchus is usually inaccessible to rigid bronchoscopes, requiring other instruments such as a flexible bronchoscope for aspirated foreign body retrieval [2]. In extreme cases, lobectomy of the lung may be needed to retrieve the foreign body [3]. In addition, if the aspirated foreign body is organic, a slippery and ungraspable surface may make the removal more difficult [1].
The Fogarty arterial embolectomy catheter was originally used for removing fresh emboli in the arterial system. However, in line with its effectiveness in removing plugged, intractable material from very narrow cavities, successful bronchial foreign body removal with a Fogarty catheter has also been reported [4,5]. However, there have been only few previous reports of the application of a Fogarty catheter in combination with a rigid bronchoscope to remove a foreign body from the left upper lobar bronchus [6,7]. In these cases, the foreign body (bead) had a central hole through which the Fogarty catheter could penetrated. Here, we present a case of left upper lobar bronchial foreign body removal in a small child. The procedure differs from previous reports, in that a plugged, unretractable left upper lobar bronchus foreign body was successfully removed using a rigid bronchoscope in conjunction with a Fogarty arterial embolectomy catheter.
CASE REPORTAn 18-month-old boy (weight, 10.5 kg; height, 79.9 cm) was brought to the pediatric emergency department due to persistent cough after eating cashew nuts at 11:00 on the same day. Upon arrival at the hospital, there was neither definite wheezing nor any signs indicating respiratory distress (i.e., cyanosis or chest retraction). Pulse oximetry showed an oxygen saturation (SpO2) of 100%. However, chest X-ray revealed hyperinflation of the left lung, suggesting a check-valve obstruction (Fig. 1). Chest computed tomography (CT) performed at another hospital showed a foreign body-like material in the left main bronchus, immediately before the division of the lobar bronchi (Fig. 1). His past medical history and laboratory results were unremarkable.
Rigid bronchoscopy was performed under general anesthesia by total intravenous anesthesia (TIVA). Induction was performed with atropine, midazolam and thiopental sodium. Then intravenous administration of lidocaine followed by continuous infusion of propofol and remifentanil was performed. Rocuronium was applied intravenously for muscle relaxation. A high-flow nasal cannula (HFNC) was applied at a flow rate of 20 L/min to support oxygenation during the whole rigid bronchoscopy procedure. The patientŌĆÖs initial SpO2 was 100% and remained stable thereafter. Under HFNC support, an initial examination was performed to locate the cashew nut pieces. A laryngoscope (8587P Benjamin-Lindholm; Karl Storz SE & Co. KG, Tuttlingen, Germany) and straight forward 0┬░ telescope (Hopkins 10324 AA; Karl Storz SE & Co. KG) were inserted up to the carina, but revealed no visible foreign body. Then, a size 4 bronchoscope was inserted (length=30 cm; Doesel-Huzly 10339 C; Karl Storz SE & Co. KG). The ventilating side port was connected to a ventilator to supply O2. Under rigid bronchoscope examination, a cashew nut piece was identified in the left main bronchus. Careful removal with grasping forceps was attempted, but due to sudden coughing of the patient, the foreign material was pushed deeper into the left upper lobar bronchus. Re-examination under rigid bronchoscopy showed that the cashew nut piece was plugging the left upper lobar bronchus (Fig. 2).
Grasping forceps was inserted, but the cashew nut piece could not be grasped due to the acute angle of the approach, which exceeded 45┬░. A basket with a ring handle (10386 AL; Karl Storz SE & Co. KG) was also introduced, but it was still not possible to retrieve the material. Finally, a 4-Fr Fogarty arterial embolectomy catheter (length=40 cm; 120404F; Edwards Lifesciences SA, Nyon, Switzerland) was inserted (Fig. 3). After placing the tip of the Fogarty arterial embolectomy catheter deeper than the cashew nut, it was inflated with a 1-cc syringe. The Fogarty catheter was slowly dragged backwards, pulling the cashew nut piece out of the left upper lobar bronchus. The Fogarty catheter was carefully pulled until the cashew nut piece and the Fogarty catheter itself were completely located within the lumen of the rigid bronchoscope. Then the rigid bronchoscope, Fogarty catheter, and cashew nut were removed together (Fig. 2).
In the final examination, the rigid bronchoscope and 0┬░ endoscope were re-inserted. After confirming the absence of residual foreign body, the patient was ventilated with a laryngeal mask airway (LMA). SpO2 remained at 99% during the remainder of the procedure. After removal of the LMA, oxygen was applied with the HFNC, at a rate of 20 L/min until the patient was fully awake and normal self-ventilation with stable SpO2 over 99% was confirmed.
The patient was discharged 1 day after the operation without any complications.
This study was approved by the Seoul National University Hospital Institutional Review Board (IRB approval number: 2106-145-1230) and was conducted in accordance with Declaration of Helsinki provisions.
DISCUSSIONThe left upper lobar bronchus lies almost perpendicular to the left main bronchus. Due to this feature of the tracheobronchial tree anatomy, an aspirated foreign body in the lower respiratory tract is rarely discovered in the left upper lobar bronchus. However, as this location is difficult to reach, removal of any foreign body located in the left upper lobar bronchus is challenging due to the poor accessibility and narrowness of the cavity. Various methods have been developed to remove foreign bodies form the left upper lobar bronchus. Cases of left upper lobar bronchus foreign body removal under fluoroscopic guidance have been reported [8]. Since the introduction of the flexible bronchoscope, many cases of successful foreign body removal under flexible bronchoscope guidance have been reported [1]. Considering the improved access to the left upper lobar bronchus conferred by its pliability, flexible bronchoscopy-guided foreign body removal from the left upper lobar bronchus has been suggested and performed [2,4]. However, to remove the foreign body with a Fogarty balloon catheter via a flexible bronchoscope, a two-stage procedure is required. First, the foreign body must be partially retrieved, to a point where it can be reached by the grasping forceps. Then, the Fogarty catheter can be withdrawn, and the grasping forceps inserted to hold and remove the foreign body. However, this two-stage procedure may be dangerous because, during retrieval with the Fogarty catheter, the foreign body may fall into the opposite main bronchus or lodge itself into the deeper segmental bronchi, which the bronchoscope and other tools cannot reach. In such cases, lobectomy of the affected lung lobe may be required to remove the foreign body [3].
Cases about airway foreign body removal with Fogarty balloon catheter have been reported. Among these cases, passingthrough technique using Fogarty balloon catheter has been reported for removal of plastic beads in a few cases [9,10]. Either with or without C-arm guidance, a Fogarty balloon catheter is passed through bronchoscope and advanced through the beadŌĆÖs opening. Then distal balloon is inflated, which enables the removal of bead as the Fogarty catheter is withdrawn. In this case, even though there was no opening within the foreign body (cashew nut) to apply this passing-through technique, due to slippery and irregular surface of the foreign body, there was a minimal gap between the lumen of the left upper lobar bronchus and the foreign body through which the Fogarty catheter could pass.
We presented a case of successful removal of a left upper lobar bronchial foreign body with a Fogarty catheter under rigid bronchoscopy guidance. In contrast to flexible bronchoscopy-guided foreign body removal, the foreign body was removed as a whole, along with the Fogarty catheter and rigid bronchoscope. Therefore, the possibility of remnant foreign body, or migration thereof, was negligible. Based on our experience in this case, we would like to emphasize that foreign bodies in the left upper lobar bronchus can be safely and effectively removed using a Fogarty arterial embolectomy catheter in combination with a rigid bronchoscope.
NOTESAuthorsŌĆÖ Contribution Conceptualization: Seong Keun Kwon. Data curation: Hyunjun Woo. Formal analysis: Hyunjun Woo, Seo Young Kim. Investigation: Hyunjun Woo, Seo Young Kim. Methodology: Hyunjun Woo, Seong Keun Kwon. Project administration: Seong Keun Kwon. Resources: Seong Keun Kwon. Supervision: Seong Keun Kwon. Visualization: Hyunjun Woo, Seo Young Kim. WritingŌĆöoriginal draft: Hyunjun Woo. WritingŌĆöreview & editing: Seong Keun Kwon. Approval of final manuscript: all authors. Fig.┬Ā1.Chest X-ray and chest CT. Antero-posterior (A) and lateral view (B) showing subtle peribronchial infiltration (circle) in left upper lobar zone. Suspicious foreign body is located at the left main bronchus (arrow), right before the division of lobar bronchi. (C) Axial view. (D) Coronal view. CT, computed tomography. 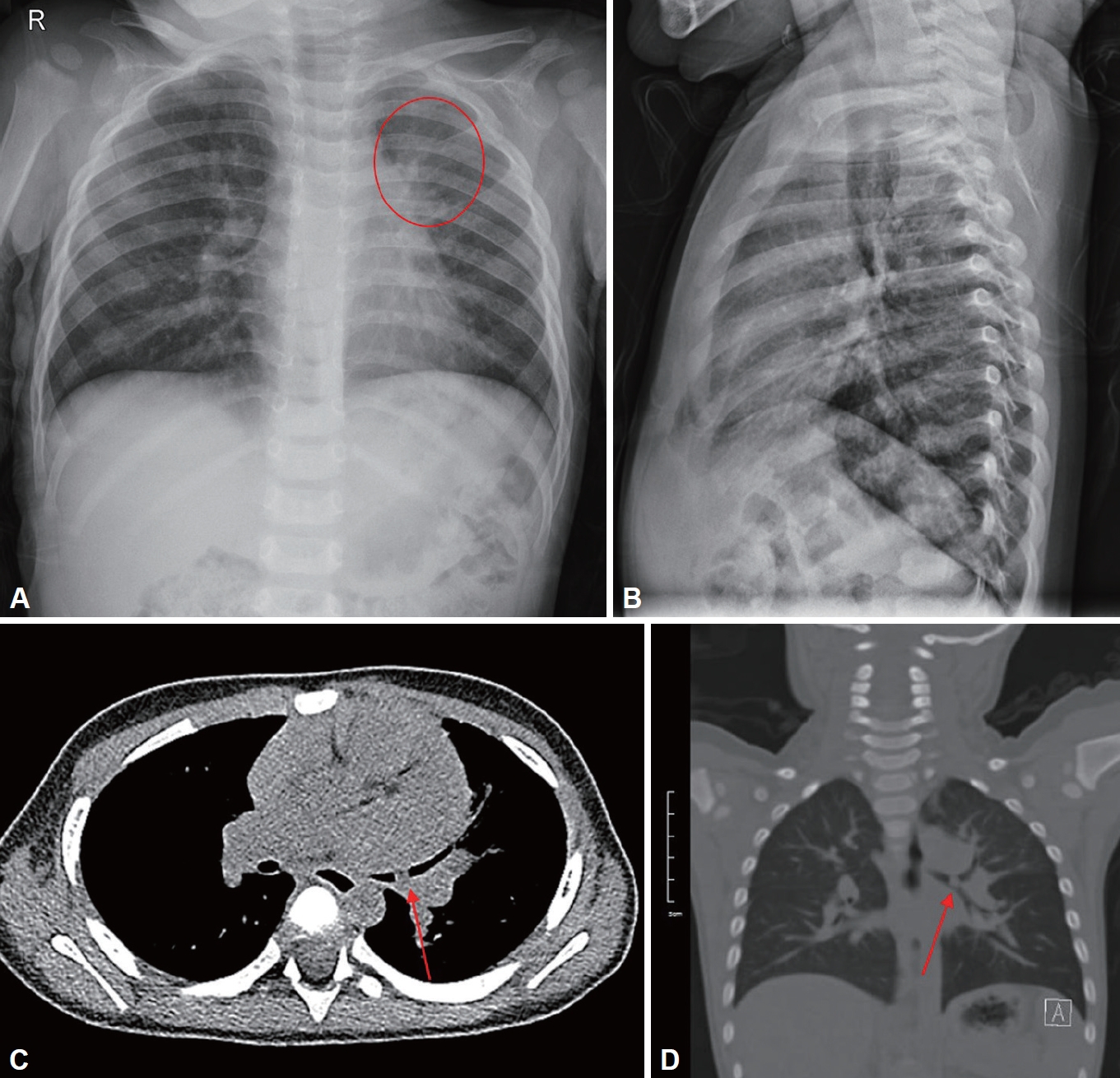
Fig.┬Ā2.Intraoperative endoscopic images and photo of extracted cashew nut. A: Cashew nut stuck at left upper lobar bronchus after patientŌĆÖs accidental coughing. B: Fogarty catheter advanced into the left upper lobar bronchus. C: After ballooning of Fogarty catheter, cashew nut being pulled out from the left upper lobar bronchus. D: Removed cashew nut. 
REFERENCES1. Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12,979 cases. Anesth Analg 2010;111(4):1016-25.
2. Akhter J, Gaspar M, Bassuk A, Roberts J. Inadvertent removal of foreign body via a flexible fiberoptic bronchoscope in a 4-year-old boy. Pediatr Pulmonol 1994;18(1):51-2.
3. Wolach B, Raz A, Weinberg J, Mikulski Y, Ben Ari J, Sadan N. Aspirated foreign bodies in the respiratory tract of children: Eleven years experience with 127 patients. Int J Pediatr Otorhinolaryngol 1994;30(1):1-10.
4. Lim SH, Lee DK, Lee JY. Bronchial foreign body removal under general anesthesia with a modified port, a fogarty balloon catheter and a grasping forceps. Korean J Anesthesiol 2011;61(2):177-9.
5. Mackle T, Russell J. The combined use of a Fogarty balloon with extraction forceps for the controlled retrieval of an endobronchial foreign body. Int J Pediatr Otorhinolaryngol 2001;60(2):163-5.
6. Landy C, Massoure PL, Gauthier J, Eve O, Kaiser E. Use of a Fogarty catheter after tracheobronchial inhalation of a bead. Trop Doct 2012;42(4):219-20.
7. Nyman AG, Krasemann TK, James P. Endobronchial foreign body removal using a coronary artery balloon catheter. J Bronchology Interv Pulmonol 2018;25(4):e50-1.
8. Hight DW, Philippart AI, Hertzler JH. The treatment of retained peripheral foreign bodies in the pediatric airway. J Pediatr Surg 1981;16(5):694-9.
|
|
|||||||||||||||||||||||||||||||||||||||