AbstractBackground and ObjectivesThe quality of life after thyroidectomy, such as voice change, is considered to be as important as control of the disease. In this study, we aimed to evaluate changes in both subjective and objective voice parameters after thyroidectomy resulting in normal morbidity of the vocal cords.
Materials and MethodIn this prospective cohort study, 204 patients who underwent thyroidectomy with or without central neck dissection at a single referral center from Feb 2015 to Aug 2016 were enrolled. All patients underwent prospective voice evaluations including both subjective and objective assessments preoperatively and then at 2 weeks, 3, 6, and 12 months postoperatively. Temporal changes of the voice parameters were analyzed.
ResultsValues of the subjective assessment tool worsened during the early postoperative follow-up period and did not recover to the preoperative values at 12 months postoperatively. The maximal phonation time gradually decreased, whereas most objective parameters, including maximal vocal pitch (MVP), reached preoperative values at 3–6 months postoperatively. The initial decrease in MVP was significantly greater in patients undergoing total thyroidectomy, and their MVP recovery time was faster than that of patients undergoing lobectomy (p=0.001). Patients whose external branch of the superior laryngeal nerve was confirmed intact by electroidentification showed no difference in recovery speed compared with patients without electroindentification (p=0.102), although the initial decrease in MVP was lower with electroidentification.
INTRODUCTIONThe worldwide prevalence of thyroid cancer has rapidly increased, and thyroidectomy is now one of the most common surgical procedures [1,2]. Because of the low mortality rate associated with thyroid cancer (papillary and follicular), the postoperative quality of life after thyroidectomy is considered to be as important as control of the disease [3]. Among the morbidities of thyroidectomy, alterations in the postoperative voice, known as post-thyroidectomy voice disorder (PTVD), reportedly occurs in 25% to 84% of thyroidectomies [4-8]. A recent survey of more than 200 post-thyroidectomy patients found that vocal changes are of more concern than common complications such as hypocalcemia or unsightly cervical scarring [9].
The presumed causes of PTVD include injury to the external branch of the superior laryngeal nerve, vascular congestion and laryngeal edema, surgical trauma to the cricothyroid muscle or cricoarytenoid joint, endotracheal intubation-related trauma, surgical adhesions, denervation of strap muscles, and pain or psychological distress [10-13]. Vocal manifestations from these various pathologies can range from a seemingly normal voice, to transient voice fatigue, or to profound and permanent dysphonia with a substantially adverse impact on the patient’s quality of life [7,8,14]. Voice changes include upper pitch loss, difficulty speaking aloud, and voice huskiness, while lowered pitch and inability to make high pitch sounds are the most common changes [8]. Although there have been several studies that have reported the results of acoustic voice analysis for post-thyroidectomy patients, few studies had sufficient power to quantify long-term outcomes [10]. In this study, we aimed to evaluate changes in voice parameters over time, which included subjective and objective assessments of patients in a single-institution, large prospective cohort study.
MATERIALS AND METHODSStudy populationThis study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 1407-074-595). From Feb 2015 to Aug 2016, patients undergoing thyroidectomy were prospectively included in this study. Informed consents were obtained from the eligible patients seen in an outpatient clinic. They underwent routine preoperative laryngeal stroboscopy and acoustic analyses, and answered a questionnaire.
During thyroidectomy, intraoperative nerve monitoring (IONM) of external branch of superior laryngeal nerve (EBSLN) was conducted. Electroidentification of the EBSLN was confirmed by cricothyroid muscle visual twitch upon stimulating with stimulating probe of NIM-Response Neuromonitoring System (Medtronic, Parkway Minneapolis, MN, USA).
After surgery, the patients making up the final cohort were enrolled according to the following criteria: 1) diagnosed with papillary thyroid carcinoma and undergoing surgery at Seoul National University Hospital, 2) staged with T1, T2, and microscopic T3 disease, 3) underwent unilateral thyroid lobectomy or total thyroidectomy with/without central neck dissection, 4) not found to have evidence of preoperative mucosal lesion or immobile vocal folds, and 5) found to have intraoperative preservation of recurrent laryngeal nerve (RLN) and postoperative normal mobility of vocal folds. The exclusion criteria were as follows: 1) stage T3 or T4 macroscopic papillary thyroid carcinoma, 2) younger than 18 years, 3) completion thyroidectomy or recurrent cancer, 4) inadvertent excision or injury of strap muscles or cricothyroid muscles, and 5) definite intraoperative injury to RLN or EBSLN.
The enrolled patients underwent follow-up examinations at 2 weeks, 3, 6, and 12 months after surgery. Laryngeal stroboscopy and acoustic analyses were performed, and a questionnaire was administered during the follow-ups.
Analysis of voice quality and assessmentUsing a comprehensive battery of functional assessments, all patients underwent repeated functional evaluations for voice quality before surgery and at 2 weeks, 3 months, 6 months, and 1 year postoperatively. In addition, all patients were given voice therapy at the same postoperative periods. The main purpose of voice therapy was to educate the possible voice change after thyroidectomy and self-exercise method.
The subjective voice outcome was assessed using visual analogue scale (VAS) score that measured defects in verbal communication with range 0–100. Although voice handicap index is useful tool for evaluating the subjective voice assessment, compliance of Korean patients to the survey decreased in long-term follow-up. Decreased reliability of time-consuming survey especially in longer postoperative duration was one of the reasons for using VAS score rather than voice handicap index. For the VAS score, a lower score indicates a greater perception of functional disability.
Voice evaluations were performed under consistent conditions by a single voice specialist who was blinded to the study. The voice specialist performed a perceptual rating of subjective voice assessments using the GRBAS scale consisting of five parameters: overall grade of hoarseness (G), roughness (R), breathiness (B), asthenia (A), and strain (S). A 4-point grading scale was used for each parameter, where 0=normal, 1=slight, 2=moderate, and 3=severe. Acoustic voice analysis was performed using the multi-dimensional voice program (MDVP) and the voice range profile (VRP) program of the computerized speech lab (CSL) for maximal vocal pitch (MVP) (Kay Elemetrics, Lincoln Park, NJ, USA). All acoustic analyses were performed with subjects in a sitting position with the microphone positioned 10 cm from their mouth. The first examination was performed using the MDVP. While recording, patients were told to voice a sustained /ah/ at a flat tone and comfortable pitch, without breaks at the same pitch for at least 4 seconds. Fundamental frequency (F0), jitter, shimmer, and noise-to-harmonics ratio (NHR) were recorded. The F0, habitual pitch, and pitch range were recorded in hertz. Jitter and shimmer were recorded in percent (%), and NHR was expressed in unique value in MDVP. The Real-Time Pitch program in CSL was used to obtain habitual pitch and voice energy. Patients read the first six sentences of the Korean standardized paragraph “Gauel (Autumn).” Pitch range was obtained by using the VRP in CSL. The patients were instructed to speak in the lowest and highest voices possible, and then to speak with progressive increase from their lowest to highest voice. The habitual pitch and pitch range were recorded in hertz, and voice energy was recorded in decibel.
The maximal phonation time (MPT) was measured using the Phonatory Aerodynamic System model 6600 (KayPENTAX, Lincoln Park, NJ, USA). During MPT measurements, patients were instructed to inhale as much air as they could and to pronounce the vowel /i/ at a normal pitch at the lowest intensity for as long as possible. The examination was run three times and the longest record was adapted.
Statistical analysesResults are presented as the mean value±standard deviation for continuous variables and as counts and group percentages for categorical variables. Continuous outcomes were analyzed using paired t tests for comparisons between two groups. For analysis of changing trend of parameters, repeated analysis of variance was used. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY, USA). p values of <0.05 were considered statistically significant.
RESULTSDemographics and clinical characteristicsA total of 204 patients were enrolled initially, and 7 patients were dropped out during the follow-up because of refusal to participate (n=1) and tumor recurrence (n=7). Finally, a total of 163 patients were enrolled in this study. Their mean age was 48.8 (19–76) years, and the male-to-female ratio was 43:161 (Table 1). Lobectomy was performed on 58 patients (28.5%) and total thyroidectomy on 146 patients (71.5%). Contact or needle-type electroidentification of the EBSLN was used in 57 patients (27.9%).
Temporal changes in postoperative voice parametersMost of the parameters showed initial aggravation followed by recovery. The subjective voice parameters, VAS and GRBAS values, showed different recovery pattern between patients with lobectomy and total thyroidectomy (Fig. 1). The differences between the VAS and GRBAS values at 2 weeks and 3 months postoperatively were significant (p<0.001, p=0.045, p=0.001, and p=0.003, respectively). Over most of the follow-up period, the patients who had undergone lobectomy showed better VAS and GRBAS values than the patients who had undergone total thyroidectomy, while the two values were about the same at 6 months and 1 year postoperatively. Jitter gradually improved 2 weeks postoperatively, while shimmer and NHR improved 3 or 6 months postoperatively (Fig. 2). Jitter at 2 weeks postoperatively in lobectomy patients was significantly worse than jitter in total thyroidectomy patients (p=0.024). MPT gradually worsened without any sign of recovery. Differences between the initial decreases in MPT and slopes of the decrease between lobectomy and total thyroidectomy patients were not significant. F0 decreased until 3 months postoperatively and then recovered in total thyroidectomy patients, while lobectomy patients showed later recovery starting 6 months postoperatively. Differences between the initial decreases in F0 at 2 weeks and 3 months postoperatively in lobectomy and total thyroidectomy patients were not significant (p=0.218 and p=0.428, respectively). MVP was significantly worse in total thyroidectomy patients than in lobectomy patients at 2 weeks and 3 months postoperatively (p=0.005 and p=0.045, respectively). However, recovery was faster in total thyroidectomy (p<0.001) and MVP at 6 months and 1 year postoperatively were about the same between patients with lobectomy and total thyroidectomy. Differences between the slopes of recovery for the lobectomy and total thyroidectomy patients for VAS, GRBAS, NHR, and MVP were significant (p<0.001, p=0.009, p=0.011, and p=0.001, respectively).
Effect of electroidentificationThe effects of electroidentification of the EBSLN on F0 and MVP in lobectomy patients were not significant compared with patients who did not undergo electroidentification (Fig. 3). In total thyroidectomy patients, the initial decreases in F0 and MVP were lower with electroidentification than in patients without, while the slopes of recovery were about the same. With regard to F0, patients with electroidentification showed significantly higher F0 at 3 and 6 months postoperatively than patients without electroidentification (p=0.030 and p=0.009, respectively). MVP at 6 months postoperatively was also significantly higher in patients with electroidentification (p=0.028). When comparing the voice parameters of patients whose EBSLN was confirmed intact by electroidentification, differences between VAS, GRBAS, jitter, shimmer, NHR, and MPT were not significant for lobectomy and total thyroidectomy patients. F0 and MVP were higher at 6 and 12 months postoperatively in total thyroidectomy patients than in lobectomy patients, although statistical significance was not attained (Fig. 4) (Supplementary Fig. 1 in the online-only Data Supplement).
DISCUSSIONThe main goal of this study was to clarify the temporal changes in the voice parameters of patients who underwent surgical treatment for thyroid cancer without apparent injury to the RLN or EBSLN. We analyzed the voice quality of patients who received surgical treatment for thyroid cancer and were stratified for analysis by the types of surgical treatment and use of electroidentification. The major findings were: 1) several voice parameters deteriorated significantly immediately after thyroid surgery; 2) these changes were more prominent in patients undergoing total thyroidectomy than in lobectomy patients and recovery occurred within 3 to 6 months.
Although most of the objective parameters recovered to the original values at 12 months postoperatively, subjective parameters, including VAS and GRBAS, did not recover to preoperative values, especially in total thyroidectomy patients. However, we have frequently encountered patients with subjective dissatisfaction with their voice, while the objective voice parameters are all within normal value. A previous report on thyroidectomy patients indicated that subjective opinions of voice after surgery were worse and lasted longer than objective parameters on voice quality would indicate [15]. Study on voice disorders suggested that patients’ subjective reports of their voice problem accurately reflected their perception of the effects of their voice problem on the functional and physiological aspects of their life, work, and social activities [16]. Therefore, an objective parameter that is assessed by a simple vowel sound and several tones should be modified to provide accurate analysis of the voice problems of patients who have undergone thyroidectomy. We think that current tools for voice analysis are insufficient for reflecting the entire aspect of patients’ subjective discomfort.
Interestingly, MPT gradually decreased without any improvement over the 12-month postoperative period. A previous study that compared the voice outcomes of patients who did not undergo thyroidectomy surgery and thyroidectomy showed that the F0, MPT, jitter, shimmer, and NHR parameters of patients not undergoing thyroidectomy were better than those of the patients who underwent thyroidectomy despite the longer operation time. Although we could not investigate the cause of decreased MPT in our study, possible explanations include the following: 1) fibrosis of the strap muscles and surrounding structures might have elicited vocal fatigue, 2) general anesthesia and decreased thyroid function might have decreased lung vital capacity, and 3) decreased F0. Further research is needed to elucidate the reasons for decreased MPT that did not improve over time, and its association with subjective parameters that did not improve.
Previous studies reported various F0 results. Some reports showed postoperative F0 values that were not significant [17,18], whereas others showed decreased F0 values [20]. A meta-analysis found significant deterioration in F0 during the early postoperative period, but not the late period [10]. With exclusion of the systematic review of approximately 850 patients, the previous studies consisted of small number of patients and were not prospective. Considering that our study was a prospective study of 204 patients at a single institution, we believe that our results on postoperative F0 are reliable and provide valuable background data for patient counseling.
In contrast, MVP significantly decreased but recovered to the preoperative value at 6 months postoperatively. As shown in Fig. 1, aggravation of most parameters was associated with surgical extent. During the early postoperative period, total thyroidectomy patients showed worse VAS and GRBAS values, jitter, shimmer, and MVP. Those differences were minimized at 6 months postoperatively, while during the late postoperative period, the differences between NHR and MPT in lobectomy versus total thyroidectomy patients were more significant. For VAS and MVP, speeds of recovery (slopes of trend) were significantly faster in total thyroidectomy patients than in lobectomy patients, but the values were about the same at 6 and 12 months postoperatively. Therefore, when the surgical extent is greater, such as for total thyroidectomy with neck dissection compared with lobectomy, patients should be informed of the possibility of early postoperative voice changes, with emphasis on the necessity of early postoperative voice therapy.
IONM has gained widespread acceptance as an adjunct to the gold standard of visual nerve identification, and IONM can be used to identify both the RLN and the EBSLN [19]. However, the number of studies that have evaluated long-term outcomes and the efficacy of electroidentification of EBSLN are limited. Studies of small numbers of patients and short follow-up periods found that electroidentification might be beneficial for both subjective and objective voice outcomes [20] Barczyński et al. [24] reported that the proportions of patients who underwent IONM for EBSLN that had decreased MPT and F0 were significantly smaller than the proportions of patients undergoing visual identification of EBSLN. Our study has strong statistical power because of the larger number of patients and longer follow-up period than other studies. Considering our study results, electroidentification should be used to minimize the decrease in MVP in patients undergoing total thyroidectomy. In contrast, electroidentification showed limited benefits for lobectomy patients. However, comparisons of the postoperative results between the lobectomy and total thyroidectomy patients who underwent electroidentification showed that all of the voice parameters were similar. We think that overall, the findings suggest that intact function of the superior laryngeal nerve as confirmed by electroidentification indicates that the vocal pitch in total thyroidectomy patients should remain equivalent to the vocal pitch of lobectomy patients.
Although, to the best of our knowledge, our study is the largest prospective cohort study to date, it has limitations. This study did not use the voice handicap index, which is widely used for the subjective assessment of voice. However, we could evaluate the trend in changes of the subjective voice outcomes with VAS. In addition, we did not use correlation analysis to assess the relationship between voice changes after thyroidectomy and quality of life. The impact of voice changes on quality of life should be evaluated to highlight the need for maintaining voice quality after thyroidectomy.
In conclusion, negative changes in voice parameters recovered over varying postoperative times, and the subjective voice measures remained significantly lower than the preoperative measures during the 12 postoperative months of follow-up. Most objective voice parameters were aggravated during the early postoperative period and recovered at 6 months, while MPT gradually decreased without any improvement at 12 months. Surgical extent seemed to be associated with voice outcomes, while the values at 12 months postoperatively between lobectomy and total thyroidectomy were about the same. Electroidentification of the EBSLN might minimize the of decrease in MVP in total thyroidectomy patients.
Supplementary MaterialsThe online-only Data Supplement is available with this article at https://doi.org/10.22469/jkslp.2022.33.2.89.
ACKNOWLEDGEMENTSThis study was supported by Seoul National University Hospital research fund (No. 2520-14-0130). The authors appreciate the medical research collaborating center at Seoul National University Hospita for data management.
NOTESAuthors’ Contribution Conceptualization: Tack-Kyun Kwon, Young Joo Park, Kyu Eun Lee. Data curation: Doh Young Lee, Goun Choe, Hanaro Park, Sungjun Han, Sung Joon Park, Seong Dong Kim, Bo Hae Kim, Young Ju Jin. Formal analysis: Doh Young Lee, Tack-Kyun Kwon. Funding acquisition: Tack-Kyun Kwon, Young Joo Park, Kyu Eun Lee. Investigation: Doh Young Lee, Tack-Kyun Kwon. Methodology: Doh Young Lee, Tack-Kyun Kwon. Project administration: Doh Young Lee, Tack-Kyun Kwon. Resources: Doh Young Lee, Tack-Kyun Kwon. Supervision: Tack-Kyun Kwon, Young Joo Park, Kyu Eun Lee. Validation: Doh Young Lee, Tack-Kyun Kwon. Visualization: Doh Young Lee, Tack-Kyun Kwon. Writing—original draft: Doh Young Lee, Tack-Kyun Kwon. Writing—review & editing: Tack-Kyun Kwon. Approval of final manuscript: all authors. Fig. 1.Changes in subjective voice assessment. Visual analogue scale (VAS) and GRBAS values were worse in total thyroidectomy at early postoperative period, while those were about the same. *Significant difference in cross-sectional comparisons between lobectomy and
total thyroidectomy patients (p<0.05). 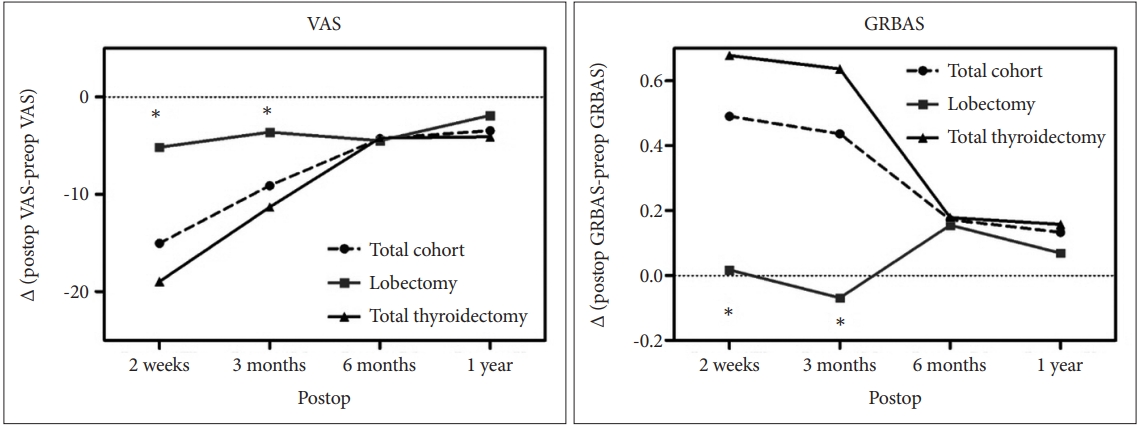
Fig. 2.Changes in acoustic analysis and voice range profiles. Differences between the slopes of recovery for the lobectomy and total thyroidectomy patients for NHR and MVP were significant (p=0.011 and p=0.001, respectively). *Significant difference in cross-sectional comparisons between lobectomy and total thyroidectomy patients (p<0.05). NHR, noise-to-harmonic ratio; MPT, maximal phonation time; MVP, maximal vocal pitch. 
Fig. 3.Change in VAS, F0, and MVP according to electroidentification of EBSLN. The effects of electroidentification of the EBSLN on F0 and MVP in lobectomy patients were not significant compared with patients who did not undergo electroidentification. *Significant difference in cross-sectional comparisons between those with and without electroidentification (p<0.05); †p-values in the graphs referred to comparisons of the slopes between those with and without electroidentification. MVP, maximal vocal pitch; EBSLN, external branch of superior laryngeal nerve. 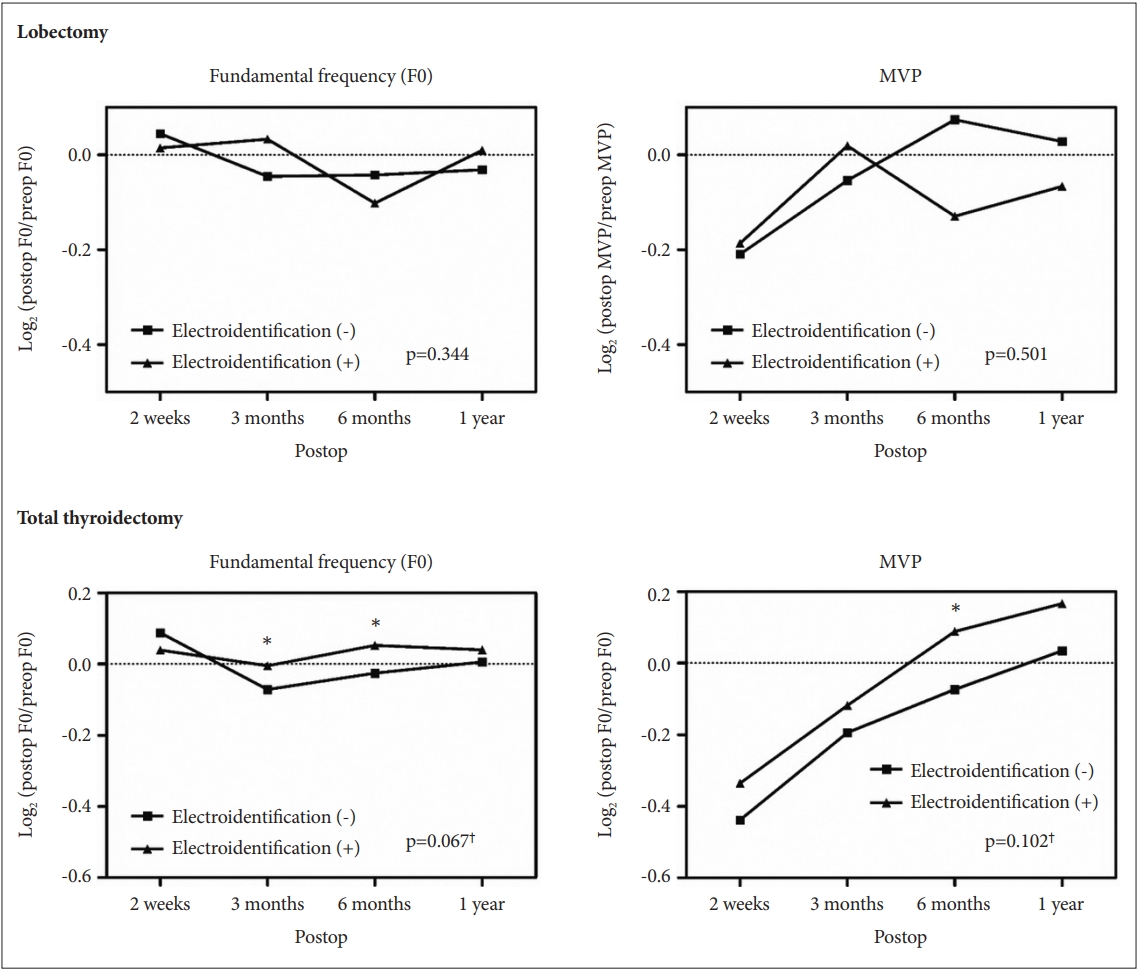
Fig. 4.Changes in F0 and MVP in patients whose superior laryngeal nerve was confirmed to be intact by electroidentification. When comparing the voice parameters of patients whose external branch of superior laryngeal nerve was confirmed intact by electroidentification, F0 and MVP were higher at postoperative months 6 and 12 in total thyroidectomy patients than in lobectomy patients, although statistical significance was not attained. †p-values in the graphs referred to comparisons of the slopes between lobectomy and total thyroidectomy patients. MVP, maximal vocal pitch. 
Table 1.Demographics and clinical/operative characteristics of cohort (n=204) REFERENCES1. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med 2000;160(4):526-34.
2. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat 2012;44(1):11-24.
3. Ryu J, Ryu YM, Jung YS, Kim SJ, Lee YJ, Lee EK, et al. Extent of thyroidectomy affects vocal and throat functions: A prospective observational study of lobectomy versus total thyroidectomy. Surgery 2013;154(3):611-20.
4. Debruyne F, Ostyn F, Delaere P, Wellens W. Acoustic analysis of the speaking voice after thyroidectomy. J Voice 1997;11(4):479-82.
5. de Pedro Netto I, Fae A, Vartanian JG, Barros AP, Correia LM, Toledo RN, et al. Voice and vocal self-assessment after thyroidectomy. Head Neck 2006;28(12):1106-14.
6. Lombardi CP, Raffaelli M, D’Alatri L, Marchese MR, Rigante M, Paludetti G, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery 2006;140(6):1026-32 discussion 1032-4.
7. Sinagra DL, Montesinos MR, Tacchi VA, Moreno JC, Falco JE, Mezzadri NA, et al. Voice changes after thyroidectomy without recurrent laryngeal nerve injury. J Am Coll Surg 2004;199(4):556-60.
8. Stojadinovic A, Shaha AR, Orlikoff RF, Nissan A, Kornak MF, Singh B, et al. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 2002;236(6):823-32.
9. Grover G, Sadler GP, Mihai R. Morbidity after thyroid surgery: Patient perspective. Laryngoscope 2013;123(9):2319-23.
10. Lang BH, Wong CK, Ma EP. A systematic review and meta-analysis on acoustic voice parameters after uncomplicated thyroidectomy. Laryngoscope 2016;126(2):528-37.
11. Teitelbaum BJ, Wenig BL. Superior laryngeal nerve injury from thyroid surgery. Head Neck 1995;17(1):36-40.
12. Soylu L, Ozbas S, Uslu HY, Kocak S. The evaluation of the causes of subjective voice disturbances after thyroid surgery. Am J Surg 2007;194(3):317-22.
13. Kark AE, Kissin MW, Auerbach R, Meikle M. Voice changes after thyroidectomy: Role of the external laryngeal nerve. Br Med J (Clin Res Ed) 1984;289(6456):1412-5.
14. Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: Improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg 2013;148(6 Suppl):S1-37.
15. Lee DY, Lee KJ, Hwang SM, Oh KH, Cho JG, Baek SK, et al. Analysis of temporal change in voice quality after thyroidectomy: Single-institution prospective study. J Voice 2017;31(2):195-201.
16. Ziwei Y, Zheng P, Pin D. Multiparameter voice assessment for voice disorder patients: A correlation analysis between objective and subjective parameters. J Voice 2014;28(6):770-4.
17. Lombardi CP, Raffaelli M, De Crea C, D’Alatri L, Maccora D, Marchese MR, et al. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery 2009;146(6):1174-81.
18. Lee J, Na KY, Kim RM, Oh Y, Lee JH, Lee J, et al. Postoperative functional voice changes after conventional open or robotic thyroidectomy: A prospective trial. Ann Surg Oncol 2012;19(9):2963-70.
|
|
||||||||||||||||||||||||||||||||||||||