AbstractForeign body (FB) aspiration remains a serious health problem, particularly in children. The complications due to occlusion by FB or related to procedures for removal can lead to morbidity and mortality. Most of the FBs are located in the unilateral bronchus, however, the organic FB can be multiple or bilaterally located when children chewed the FB. Here, we present a case of successful retrieval of bilateral bronchial FBs. Preoperatively, FB in the left main bronchus was diagnosed, however, FB of the right upper bronchus was not definitive on X-ray and CT scan. During the rigid bronchoscopy, occult FB in the right upper bronchus was detected and successfully removed.
INTRODUCTIONForeign body (FB) aspiration into the tracheobronchial tree is a significant cause of morbidity and mortality in pediatric patients and continues to be a challenge for the otolaryngologist despite significant advances in prevention, first aid, and endoscopic technology [1,2]. The peak age of incidence is between 1 and 3-year-old and organic FB is more prevalent, dominated by peanuts [3]. Many organic FB can be aspirated at once [4], and one FB can be fragmented because the children can chew the food materials. For this reason, FB can be multiple and bilateral, however, bilateral bronchial FB is a rare condition and difficult to identify preoperatively and can be life-threatening if the complete FB retrieval is failed. Here, we present a case of a 20-month-old boy with bilateral bronchial FB which was successfully removed by endoscopy-assisted rigid bronchoscopy.
CASE REPORTA 20-month-old boy with a 6-day history of FB aspiration was referred to our hospital for further evaluation. The FB was chewed walnut by history taking and he showed a wheezing sound with a mild cough. There was a wheezing sound with decreased breath sound on his left chest at physical examination.
Chest radiography visualized hyperinflation of the left lung, displacement to the right side of the mediastinal structure, and atelectasis of the right upper lung zone (Fig. 1A). To determine the existence and location of the FB, low-dose chest CT was performed, and CT showed foreign material in the left main bronchus; the left main bronchus was almost completely occluded and the right main bronchus seemed to be not obstructive (Fig. 1B and C). A rigid bronchoscopic FB retrieval was requested for the retrieval of a FB.
Under general anesthesia, rigid bronchoscopy (internal diameter 3.5 mm, Karl Storz GMBH & Co., Tuttlingen, Germany) with a 2.3 mm endoscope (Karl Storz GMBH & Co.) was intubated to the trachea (Fig. 2A and B). Under endoscopic guidance, bilateral bronchial FBs were separately identified which are lodged in the left main bronchus (size 6 mm) and right upper lobar bronchus (4 mm) (Fig. 2C and D). The FBs were successfully extracted by rigid forceps under endoscopy-assisted rigid bronchoscopy (Fig. 2C) and we confirmed that there was no remnant FB fragment in both bronchi (Fig. 2E and F) and recovery of the breath sound on both lungs.
The patient recovered well without any symptoms and signs of pulmonary complications and follow-up chest radiography showed no evidence of abnormal features (Fig. 3). He was discharged 4 days after the operation.
DISCUSSIONFB aspiration happens because children commonly have various objects or food in their mouth while playing, running, crying, laughing, or coughing, thus increasing the possibility of making a forced inspiring movement [5]. According to the literature and recent study, tracheobronchial FB was often unilateral and located in the right bronchial due to the anatomic angle, the right main bronchus being shorter and wider, as an extension of the trachea [3,6]. As we have seen in our case, it is a rare case of FBs that lodge in bilateral bronchi which was underdiagnosed preoperatively. Bilateral FB could be identified and removed because of our policy that the whole bronchial tree should be evaluated during bronchoscopic FB retrieval even though the patients with bilateral bronchial FBs tend to be desaturated quickly compared to unilateral FB patients.
The types of bronchial FB are variegated, depending on patient age and cultural background including religious beliefs as well as alimentary habits [7]. Bronchial FB can be multiple especially when children can chew the food materials and physicians should be concerned about the undetected FB which can be the cause of recovery delay after retrieval. Bilateral bronchial FB was reported at about 1.9% [3], and only one case was reported in Korean literature [8].
Chest radiography provides important information to the physician. The most common findings were mediastinum swing, emphysema, and atelectasis [9]. Common false-negative radiographs, however, cannot exclude the presence of FBs in the airways. In this instance, CT may help diagnose and in determining the exact existence and location of the FB in patients [10,11]. The chest radiography, in this case, visualized hyperinflation of the left lung, displacement to the right side of the mediastinal structure, and atelectasis of the right upper lung zone. The possibility of FB in the right upper bronchus was not concerned preoperatively because CT showed no definitive foreign material in the right bronchus. In this aspect, CT seems to be not helpful especially when FB is smaller than CT section thickness.
The removal of an FB can be performed with flexible or rigid bronchoscopy [12]. The selection of the endoscopic material depends on the physicianŌĆÖs preference. Some teams use flexible bronchoscope with the removal of substantially all FB, while most authors consider that rigid bronchoscope is a very safe and effective procedure in treating such patients [3]. We use a bimanual endoscope-assisted rigid bronchoscopy method which was reported as superior to the conventional naked eye method [13]. In addition, after FB removal, the patency of the tracheobronchial tree and remnant FB can be carefully examined with the magnified view by endoscopy-assisted rigid bronchoscopy. Our experience suggests that bilateral bronchi should be examined during bronchoscopic FB retrieval before and after surgery for conviction of remnant or undetected FB.
NOTESAuthorsŌĆÖ Contribution Conceptualization: Sungchul Ko, Ki Nam Park. Data curation: Jaeha Lee, Sothearith Loek. Formal analysis: Jaeha Lee, Sothearith Loek. Funding acquisition: Ki Nam Park. Methodology: Sungchul Ko, Ki Nam Park. Project administration: Sungchul Ko. Resources: Sothearith Loek, Ki Nam Park. Supervision: Ki Nam Park. Validation: Ki Nam Park. WritingŌĆöoriginal draft: Sungchul Ko. WritingŌĆö review & editing: all authors. Approval of final manuscript: all authors. Fig.┬Ā1.Preoperative radiologic evaluation. Chest radiography showed hyperinflation of the left lung and suspicious atelectasis of the right upper lung zone (A). The chest CT showed a foreign body (FB) in the left main bronchus (B) and suspicious FB in the right upper lobar bronchus (C). 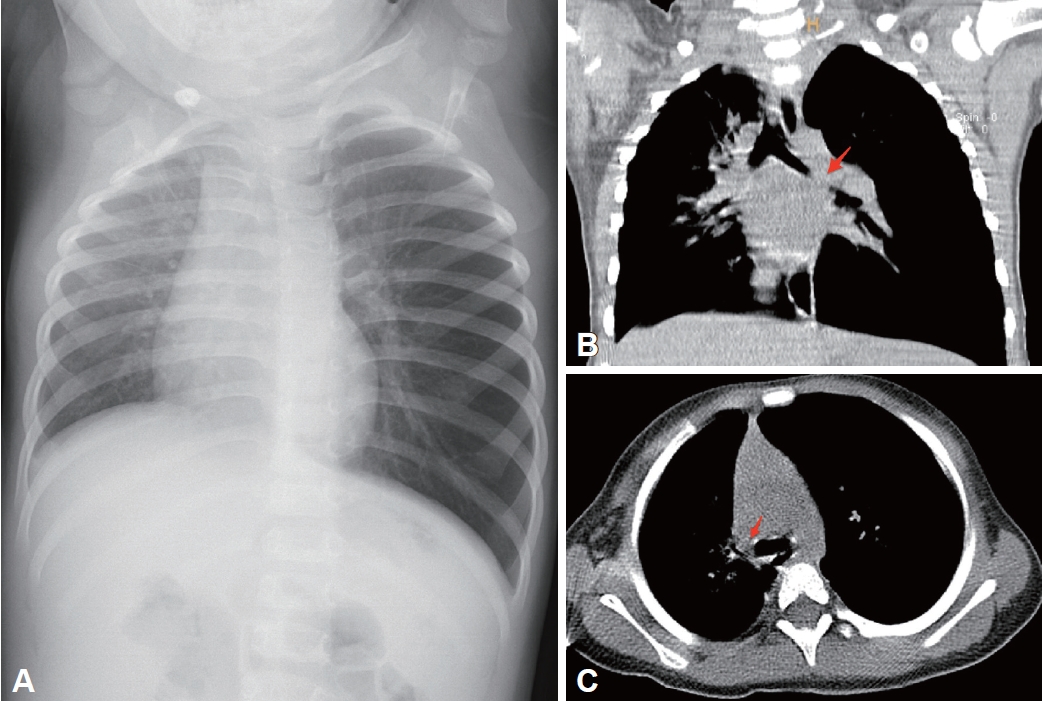
Fig.┬Ā2.Rigid bronchoscopic retrieval of bilateral bronchial FBs. The ventilating bronchoscopy with a 3.5 mm inner diameter was used and the whole procedure was carried out under endoscopic visualization. After the insertion through the vocal cords (A), ventilation via bronchoscopy was applied after the identification of successful insertion into the trachea (B). The FB in the left main bronchus was identified and removed (C). After the removal of the left FB, the air passage and no remnant FB were identified (D). During the whole bronchial tree evaluation, right upper bronchial FB was identified and could be removed (E). After retrieval of right FB, patency of bronchus and scanty bleeding were identified (F). FB, foreign body. 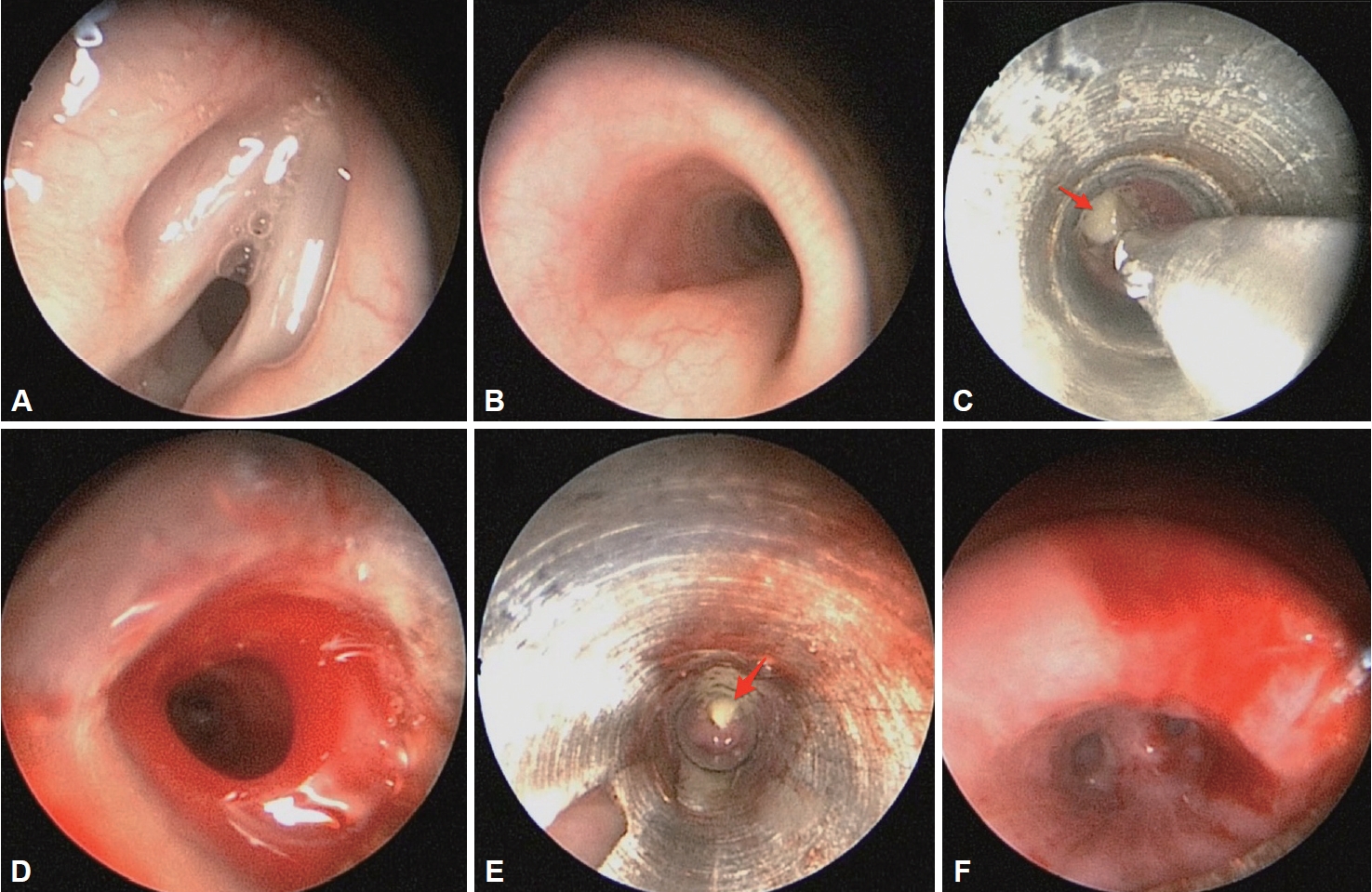
REFERENCES1. Kaur K, Sonkhya N, Bapna AS. Foreign bodies in the tracheobronchial tree: A prospective study of fifty cases. Indian J Otolaryngol Head Neck Surg 2002;54(1):30-4.
2. Eren S, Balci AE, Dikici B, Doblan M, Eren MN. Foreign body aspiration in children: Experience of 1160 cases. Ann Trop Paediatr 2003;23(1):31-7.
3. Boufersaoui A, Smati L, Benhalla KN, Boukari R, Smail S, Anik K, et al. Foreign body aspiration in children: Experience from 2624 patients. Int J Pediatr Otorhinolaryngol 2013;77(10):1683-8.
4. Sih T, Bunnag C, Ballali S, Lauriello M, Bellussi L, et al. Nuts and seed: A natural yet dangerous foreign body. Int J Pediatr Otorhinolaryngol 2012;76 Suppl 1:S49-52.
5. Skoulakis CE, Doxas PG, Papadakis CE, Proimos E, Christodoulou P, Bizakis JG, et al. Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int J Pediatr Otorhinolaryngol 2000;53(2):143-8.
6. Zhijun C, Fugao Z, Niankai Z, Jingjing C. Therapeutic experience from 1428 patients with pediatric tracheobronchial foreign body. J Pediatr Surg 2008;43(4):718-21.
7. Szafrański W, Dobielski J, Papiewski W, Czechowska U. [Occult bronchial foreign bodies - analysis of own material]. Pneumonol Alergol Pol 2013;81(1):40-4.
8. Kwoen OK, Chon JY, Kim ES, Ahn BI. Anesthesia for removal of foreign bodies in bilateral main bronchi. Korean J Anesthesiol 1995;28(1):181-5.
9. Tang FL, Chen MZ, Du ZL, Zou CC, Zhao YZ. Fibrobronchoscopic treatment of foreign body aspiration in children: An experience of 5 years in Hangzhou City, China. J Pediatr Surg 2006;41(1):e1-5.
10. Bai W, Zhou X, Gao X, Shao C, Califano JA, Ha PK. Value of chest CT in the diagnosis and management of tracheobronchial foreign bodies. Pediatr Int 2011;53(4):515-8.
11. Lin CY, Huang SF, Lan CC, Wu YK, Huang CY, Huang YC, et al. Fish fin aspiration: An unusual type of lower airway foreign body in a Chinese adult. Respir Care 2013;58(3):e20-2.
|
|
||||||||||||||||||||||||||||||||||||||||||