AbstractA 16-year-old girl was incidentally found to have a mediastinal lipogenic mass, which was confirmed as a hibernoma on biopsy. Mediastinal mass excision with full sternotomy was performed, and follow-up chest computed tomography at postoperative 1 year revealed a residual or recurred mass at the left neck (level VI). Consequently, left level-VI neck dissection was performed, and the biopsy also confirmed hibernoma. During neck dissection, an electromyography tube was used to monitor the recurrent laryngeal nerve, and complete removal was achieved without damage to the vagus nerve, carotid vessels, or thyroid gland. When managing cervical lipogenic tumors, clinical suspicion is necessary, followed by radiological and pathological evaluations to differentiate malignancies. If a hibernoma is suspected, en bloc resection of the tumor is crucial to prevent hemorrhage and recurrence. Cervical hibernoma can cause symptoms such as dysphagia, weight loss, and exertional dyspnea owing to its mass effect. Surgeons should be cautious during tumor removal to protect the recurrent laryngeal nerve. We successfully removed the residual or recurred hibernoma in the neck without complications.
INTRODUCTIONHibernomas are rare, benign lipogenic tumors. Hibernomas occurring in the head and neck are even rarer, with only a few cases reported in the literature. Clinical suspicion is of primary importance in the management of patients with lipogenic tumors, followed by histological and imaging evaluations to rule out lipomatous malignancies. Surgical removal of a cervical hibernoma is needed when it causes symptoms such as dyspnea or dysphagia due to its mass effect or when malignancy cannot be excluded. During surgery, en bloc resection is crucial to prevent hemorrhage and recurrence, and preservation of the recurrent laryngeal nerve is important. We describe the successful removal of a residual or recurred hibernoma in the neck.
CASE REPORTA 16-year-old girl was incidentally found to have mediastinal widening in plain chest radiography during a medical examination. She was referred to the department of thoracic surgery on April 10, 2019. The patient denied any underlying diseases or family history of malignancy, and had no history of smoking or alcohol consumption. She presented with symptoms of dysphagia, weight loss, and exertional dyspnea during her initial visit; however, her symptoms were not severe and were neglected until plain chest radiography was performed. Her initial height and weight were 160 cm and 42.5 kg, respectively.
Chest computed tomography (CT) revealed a fat-containing mass lesion without calcification in the lower neck extending to the posterior upper mediastinum, measuring approximately 9.5├Ś6.1 cm, and tracheal compression was observed. The differential diagnosis made by a radiologist was well-differentiated liposarcoma or immature teratoma. Further evaluation using positron emission tomography (PET)/CT revealed mild uptake (~1.9) in the mass, with metabolic defects in the fat portion (Fig. 1). Core needle biopsy confirmed a lipogenic tumor with brown fat cells, suggestive of a hibernoma.
The thoracic surgery team excised the mediastinal mass via full sternotomy with veno-venous extracorporeal membrane oxygenation (V-V ECMO) support. The anesthesiologist recommended V-V ECMO support due to >50% mid-tracheal compression with a diameter of <5 mm, through which only a 3.0-mm endotracheal tube could barely pass. Prior to anesthesia induction, a fiberoptic rigid bronchoscope was prepared and a high-flow nasal cannula was applied as a precaution for possible emergent airway collapse. Under monitored anesthesia care, V-V ECMO was inserted with 17-Fr catheters in the right and left femoral veins, followed by general anesthesia with endotracheal intubation using a 6.5-mm plain tube. The intubation was uneventful, with an intubation depth of 22 cm, and airway patency was confirmed using fiberoptic bronchoscopy.
During the main surgical procedure, a full median sternotomy approach was used, and a large, well-circumscribed, lobulated mass was identified in the superior aspect of the anterior mediastinum extending to the anterior neck. Adhesion to nearby tissues was minimal, and there was no evidence of vessel, nerve, or pleural invasion. Delicate dissection was performed and the mass was completely removed while preserving the bilateral recurrent laryngeal nerves. The patient was transferred to the pediatric intensive care unit after surgery and was discharged on postoperative day 5 without complications.
The size of the mediastinal mass was 9.6├Ś7.9├Ś3.8 cm, and the final pathology confirmed the diagnosis of mediastinal hibernoma. On gross examination, the resected mediastinal lesion contained a fatty tissue-like yellowish mass measuring 5.3 cm. The mass was composed of polygonal cells resembling brown fat with multivacuolated cytoplasm and admixed with mature adipocytes. The lesion was also characterized by fibrous septa and myxoid stroma, suggesting the presence of a myxoid variant. Small, delicate branching capillaries were observed. The nuclei were small with no significant atypia, and necrosis was not observed. Immunohistochemistry for CD31 revealed hibernoma and capillary endothelial staining (Fig. 2).
Regular follow-up was conducted using posteroanterior chest radiography, with no evidence of recurrence. The initial symptoms, such as dysphagia and dyspnea, disappeared, and she had no complaints. She had also gained weight, and her body weight was 47.4 kg on January 10, 2022. However, chest CT taken on August 26, 2020 and September 1, 2021 showed a small, growing lesion (1.3 cm to 2.2 cm) with attenuating features in the left supraclavicular area, which was suspicious for residual mass or recurrence (Fig. 3). Owing to its location, the patient was referred to the otolaryngology department.
The patient denied any subjective symptoms; however, a left level-VI neck dissection was performed on January 25, 2022, as the mass continued to grow. An electromyography tube was inserted for intraoperative recurrent laryngeal nerve monitoring. A midline horizontal incision of 5 cm was made along the skin crease at the level of the thyroid gland. During the removal process, the mass was well-circumscribed with a capsule, and pinpoint capsule violation was observed; however, there was no definite spillage of the tumor content. A delicate dissection was performed to preserve nearby structures (Fig. 4). Eventually, complete removal was achieved, and the left vagus nerve, carotid vessels, and thyroid gland were preserved. The left recurrent laryngeal nerve could not be identified because of severe adhesions; however, the patientŌĆÖs vocal fold movement was intact postoperatively. The tumor at the left level VI was also confirmed as a hibernoma with clear resection margins, which had similar histologic features with more pronounced myxoid stroma than the mediastinal mass (Fig. 2).
The patient was discharged on postoperative day 2 without complications, including vocal fold palsy. There was no evidence of recurrence on the 6-month follow-up neck CT scan. Further monitoring for recurrence will continue.
DISCUSSIONA hibernoma is a rare, benign tumor that consists of cells that histologically resemble brown fat cells [1]. It was first named ŌĆ£hibernomaŌĆØ by Grey in 1914 because of its histological similarity to the brown fat of hibernating animals [2]. Unlike typical adipose tissue, brown fat has abundant vascularity that generate heat [3]. Brown fat usually disappears after eight weeks of life, and is slowly replaced by white fat [4].
Hibernomas account for only 1% of all benign lipomatous tumors and are usually asymptomatic unless they compress nearby structures. It is most commonly identified in the thigh, but can also occur anywhere with scattered brown fat, such as the bone, scalp, neck, axilla, shoulder, thorax, breast, and stomach [2]. Its prevalence peaks in the fourth and fifth decades of life, and its sex predominance is controversial [3,4].
Due to its low incidence, hibernomas are sometimes misdiagnosed as liposarcomas. On CT, hibernomas may present as well-circumscribed hypodense lesions with linear septations, indicating high vascularity [3]. On magnetic resonance imaging (MRI), hibernomas can be isointense or relatively hypointense to the surrounding fat on both T1 and T2, and diffuse heterogeneous enhancement can be identified due to the hypervascularity of the mass. On PET/CT, hibernomas show uptake due to metabolically active brown fat tissue. However, none of the images listed above are pathognomonic, which can hinder the differentiation of hibernomas from sarcomas [2].
Therefore, pathological diagnosis should be performed before the initial treatment to exclude malignancy. Fine needle aspiration is suggested over core needle biopsy, as there is a possibility of hemorrhage due to the high vascularity of the hibernoma. However, some prefer core needle biopsy because sufficient tissue can increase diagnostic yield [2].
As described in this case, large multivaculolated brown fat cells, single central or small eccentric nuclei, large amount of granular cytoplasm, fibrous septa, and branching capillaries can be observed upon microscopic examination of hibernoma [2].
Furlong et al. [5] suggested four main histological variants of hibernoma: typical, spindle, lipoma-like, and myxoid. Typical hibernoma and lipoma-like variants occur most commonly in the thigh, whereas myxoid and spindle cell types are frequently found in the head and neck regions. Typical hibernomas, characterized by eosinophilic, pale, and myxoid cells, account for approximately 82% of all cases. The second most common type is the myxoid variant, which has a loose basophilic matrix and accounts for 9% of all cases. The lipoma-like and spindle cell types accounted for 7% and 2% of all cases, respectively. However, most surgical pathologists do not subclassify these subtypes because they have similar prognosis [2].
Because of its multiple pathological variants and the possibility of misdiagnosis, regardless of clinical, imaging, and pathological information, some researchers have suggested additional chromosomal evaluation to differentiate hibernomas [1].
To date, there have been no reported cases of malignant transformation or metastasis of hibernoma; therefore, theoretically, asymptomatic hibernoma does not require treatment [5]. However, because of the diagnostic uncertainty of the modalities mentioned above, en bloc resection of the mass is the treatment of choice. En bloc removal is important for preventing recurrence and bleeding due to its high vascularity. According to previous studies, almost none of the patients with hibernoma had disease recurrence and none died due to complications of hibernoma with en bloc resection. Some exceptions with recurrences were possibly due to positive resection margins rather than true recurrence [2].
In this case, because hibernoma is well known for having no recurrence after complete removal, the residual or recurred hibernoma may have been a result of a remnant tumor after the first surgery, despite clear resection margins. It would have been desirable to have a collaborative approach between the Departments of Thoracic Surgery and Otolaryngology for the first surgery, considering the mass extension from the thoracic cage to the infrathyroid level on the initial CT. In addition, although vocal fold palsy did not occur in this patient, it was difficult to identify the recurrent laryngeal nerve during the second surgery because of adhesions caused by the first surgery. Therefore, to prevent recurrence and complications of hibernomas, complete removal should be achieved during the initial surgery.
Fig.┬Ā1.Initial imaging. A: Axial chest CT. B: Coronal chest CT. C: PET/CT. D: Ultrasound showing mass from lower neck to posterior upper mediastinum. The ultrasound showed a well-circumscribed heterogenous mass with increased vascularity. PET/CT, positron emission tomography/computed tomography. 
Fig.┬Ā2.Pathologic review of the mass. A: The lesion was a fatty tissue-like yellowish mass on gross examination. B: Polygonal cells resembling brown fat with multivacuolated cytoplasm were admixed with mature adipocytes in the background of myxoid stroma. C: Small, delicate, branching capillaries were noted. D: No significant nuclear atypism was seen. E: CD31 immunostaining highlighted hibernoma cells and capillary endothelial cells. F: The residual or recurred tumor in the supraclavicular area had similar histologic features with more pronounced myxoid stroma. 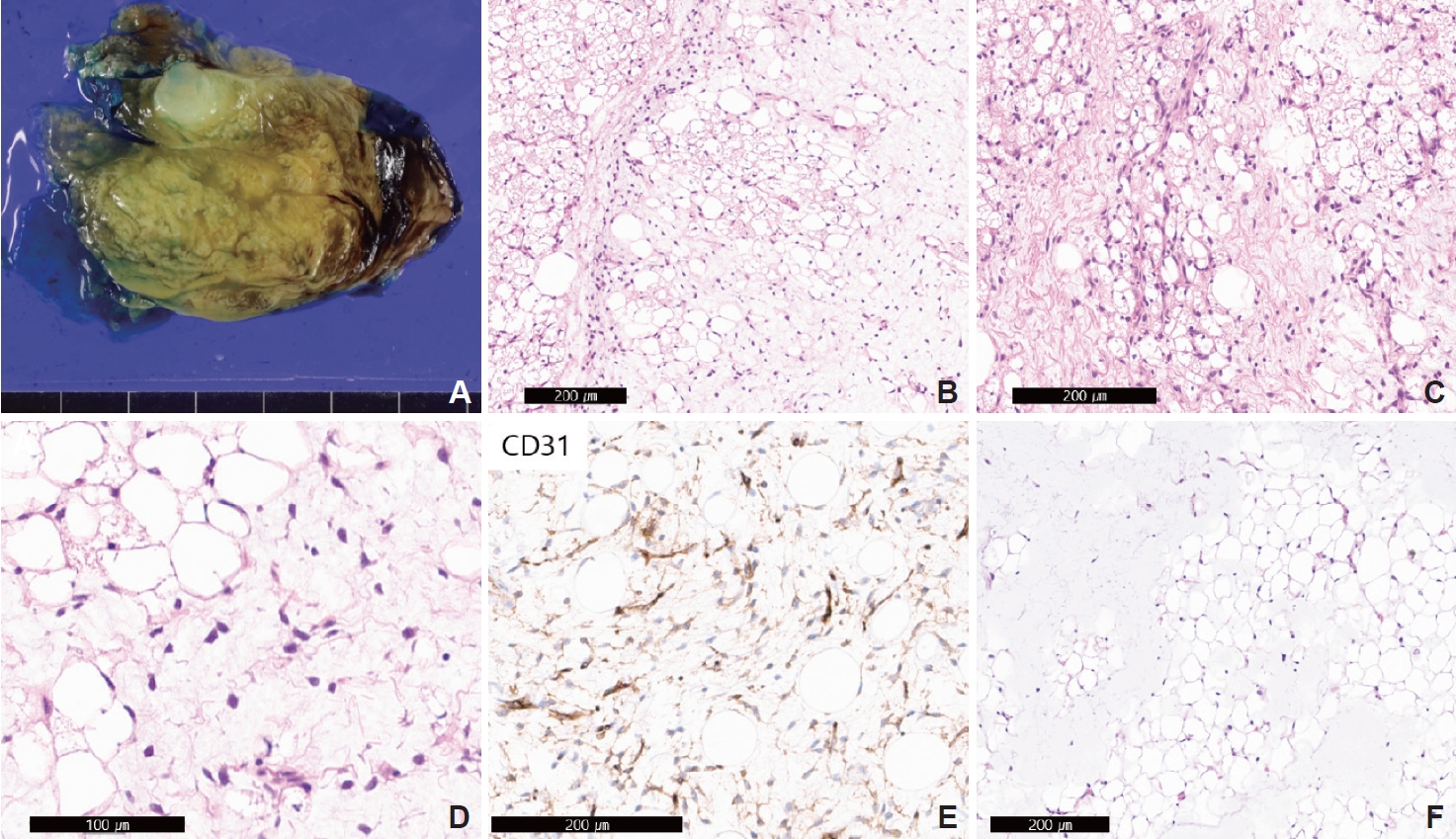
Fig.┬Ā3.Chest CT showing residual or recurred tumor at left supraclavicular area (red arrows). A: Axial view of chest CT on August 26, 2020. B: Coronal view of chest CT on August 26, 2020. C: Axial view of Chest CT on September 1, 2021. D: Coronal view of chest CT on September 1, 2021. 
Fig.┬Ā4.. Intraoperational photo of left supraclavicular residual or recurred hibernoma. A: The hibernoma (left arrow) was well circumscribed with a capsule at the inferior side of the left thyroid gland (right arrow). Delicate dissection was performed to save nearby structures. B: Anterior plane of removed hibernoma. C: Posterior plane of removed hibernoma. I, inferior; L, lateral; M, medial; S, superior side of the patient. 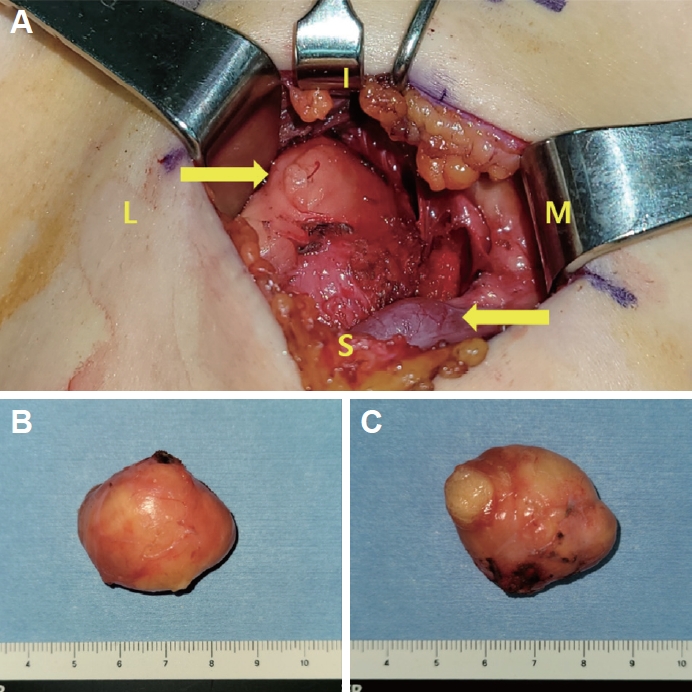
REFERENCES1. Turaga KK, Silva-Lopez E, Sanger WG, Nelson M, Hunter WJ, Miettinen M, et al. A (9;11)(q34;q13) translocation in a hibernoma. Cancer Genet Cytogenet 2006;170(2):163-6.
2. AlQattan AS, Al Abdrabalnabi AA, Al Duhileb MA, Ewies T, Mashhour M, Abbas A. A diagnostic dilemma of a subcutaneous hibernoma: case report. Am J Case Rep 2020;21:e921447.
3. Prendes BL, Kohli C, Brooks JS, Newman JG. Cervical hibernoma, a rare, benign tumor: case report. Ear Nose Throat J 2011;90(1):E19-21.
|
|
||||||||||||||||||||||||||||||||||||||||